Assessment of Peripancreatic Fat Infiltration of Pancreatic Ductal Adenocarcinoma by Multidetector-Row Computed Tomography: Correlation to Extrapancreatic Nerve Invasion and Surgical Outcomes
Yusuke Yamamoto*1, Kazuaki Shimada1, Takeuchi Yoshito2, Hata Syojiro1, Satoshi Nara1, Minoru Esaki1, Yoshihiro Sakamoto1, Tomoo Kosuge1, Nobuyoshi Hiraoka3
1Hepatobiliary and Pancreatic Surgery, National Cancer Center Hospital, Tokyo, Japan; 2Diagnostic Radiology Division, National Cancer Center Central Hospital, Tokyo, Japan; 3Pathology Division, National Cancer Center Research Institute, Tokyo, Japan
Background: Retroperitoneal invasion including extrapancreatic nerve plexus invasion of pancreatic ductal adenocarcinoma, which has been demonstrated as peripancreatic fat infiltration by multidetector-row computed tomography (MDCT), is a distinct characteristic associated with unresectability and impaired survival after surgery. The aim of this study was to investigate whether the degree of peripancreatic fat infiltration determined by MDCT is a useful predictor of surgical outcomes in patients with pancreatic ductal carcinoma.Patients and methods: The clinical records of 132 patients that underwent macroscopic curative pancreaticoduodenectomy for pancreatic adenocarcinoma between January 2004 and December 2008 were reviewed retrospectively. The MDCT scan acquired in all patients were reviewed in consensus by two abdominal radiologists. Peripancreatic fat infiltration was determined and classified by MDCT into 4 groups to the following grade: grade 0, no peripancreatic fat infiltration; grade 1, a strand or streak structure radiating from the tumor (< 5 mm); grade 2, a strand or streak structure radiating from the tumor without abutting the major artery (> 5 mm); grade 3, a streak structure radiating from a tumor and abutting to a major artery. The clinicopathologic factors including the grade of peripancreatic fat infiltration as potentially important predictors for survival were analyzed. The relationship of the grade of peripancreatic fat infiltration and various histopathologic factors were also investigated.Results: The incidence of peripancreatic fat invasion was as follows: grade 0, n = 8 (6%); grade 1, n = 54 (41%); grade 2, n = 49 (37%); grade 3, n = 21 (16%). Five-year survival rate was 55.6% for grade 0, 38.7 % for grade 1, 16.4% for grade 2, and 0% for grade 3, respectively. There were significant differences in the survival rates between grade 1 and 2 (p = 0.003), and grade 2 and 3 (p = 0.032), respectively. Multivariate survival analysis showed that lymph node metastasis, surgical margin positive, and grade 2 and 3 pancreatic far infiltration were independently associated with a poorer prognosis. Only extrapancreatic nerve plexus invasion was significantly associated with grade 2 and 3 pancreatic fat infiltration. Conclusion: The grade of peripancreatic fat infiltration determined by MDCT, which was significantly related with the incidence of histological extrapancreatic nerve plexus invasion, may be useful as a predictor for survival after pancreaticoduodenectomy in patients with invasive ductal carcinoma of the pancreas.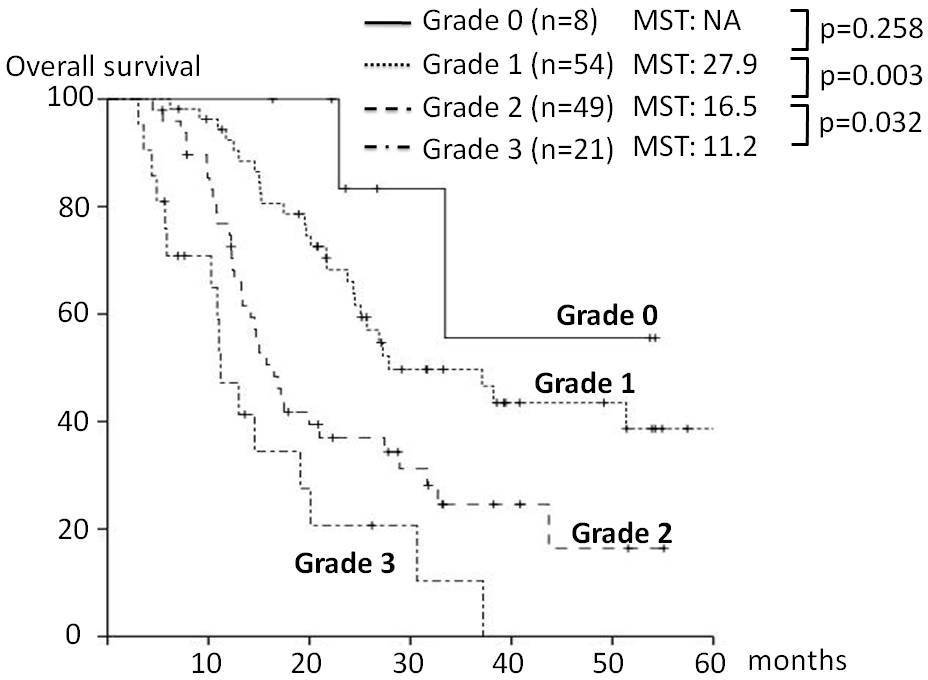
Back to 2011 Program



