Assessing Quality of Life in Pancreatic Cancer: a Shifting Landscape
Jillian K. Smith*, Jessica P. Simons, Elan R. Witkowski, Andreea Bodnari, Mary Beth Curnen, Sing Chau NG, Mary E. Sullivan, Shauneen Valliere, Shimul a. Shah, Jennifer F. Tseng
Surgical Outcomes Analysis & Research, Dept. of Surgery, University of Massachusetts Medical School, Worcester, MA
BACKGROUND: Pancreatic cancer is a devastating disease with five-year survival of <5%; thus, additional outcome measures accounting for quality of life (QOL) and functional status become increasingly important. Little is understood, however, about QOL in living with pancreatic cancer and undergoing treatment, including surgery. Decision-making for patients is frequently influenced by stakeholders such as family members, healthcare professionals, or even patients themselves who are not currently experiencing the health state of interest, e.g. post-operative recovery. We sought to determine how educated stakeholders evaluated QOL with pancreatic cancer, and to compare these measured perceptions with directly assessed QOL of patients throughout diagnosis and treatment.METHODS: First, stakeholder opinions on pancreatic cancer diagnosis and treatment were gathered via anonymous simultaneous polling using TurningPoint 4.2.3 software in November 2010 during a pancreatic cancer symposium. Respondents included patients, family, and healthcare professionals. Second, individual patient assessments of QOL were conducted by trained physicians using the EORTC QLQ-C30 and PAN26 standardized surveys administered to patients at initial clinic appointment with surgical oncologist and follow-up appointments from November 2007 through May 2009.RESULTS: Stakeholders (n=65) included nurses (n=24), family members of patients with pancreatic cancer (n=13), pancreatic cancer survivors (n=5), physicians (n=5), and other, including scientists (n=18). Regarding general stakeholder perceptions of living with pancreatic cancer, the mean rank for overall QOL was 4.8/10 (scale 0-10, 10=perfect health); for immediately post-operative was 4.1/10; and for 6 months post-operative was 5.7/10 (Figure). Individual pancreatic cancer patients (n=12), in contrast, demonstrated a mean global QOL score of 58% preoperatively, 72% immediately post-operatively, and 63% >3 months from surgery (Figure). Intriguingly, the individual functional scales demonstrated improvement after the immediate post-operative period over the time studied, which correlated with the stakeholders’ survey; however, the overall individual patient-assessed QOL showed a paradoxical decline after this period.CONCLUSIONS: Overall quality of life of pancreatic cancer patients appears to initially improve following surgery, but then declines, despite improvement in functional status seen across multiple scales. Our data suggest that the opinions of stakeholders, including patients further removed from diagnosis and surgery, do not reflect the perceptions of patients actually living through the surgical treatment of pancreatic cancer. As QOL and functional status become increasingly important in assessing outcomes for cancer patients, additional investigation into the quantification and definition of QOL is warranted.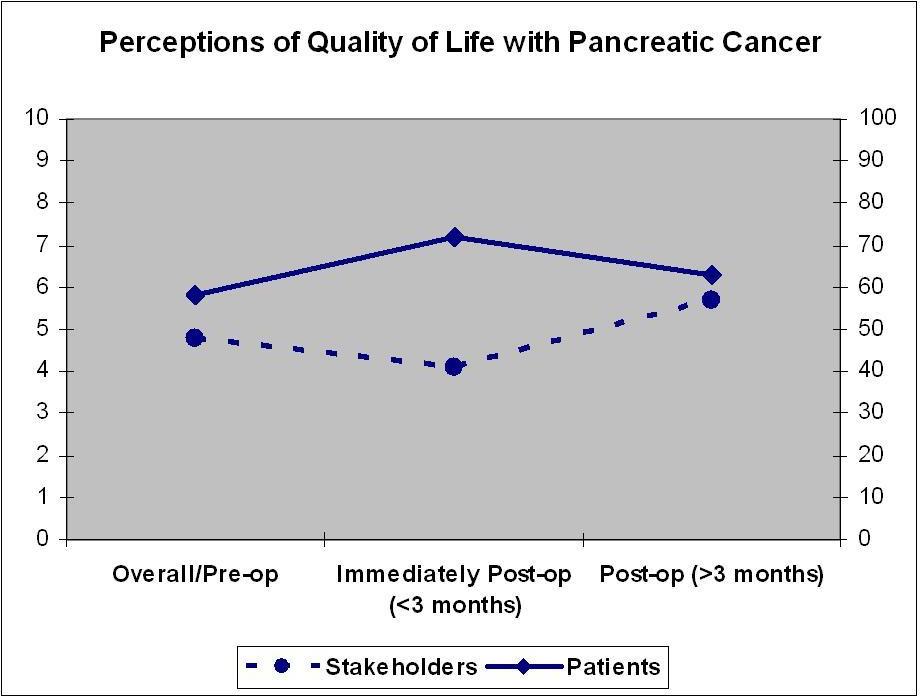
Back to 2011 Program



