The Impact of Regionalization of Pancreaticoduodenectomy for Pancreatic Cancer in North Carolina Since 2004
Ryan Z. Swan*, David Sindram, Amanda Walters, John B. Martinie, David a. Iannitti
Surgery, Carolinas Medical Center, Charlotte, NC
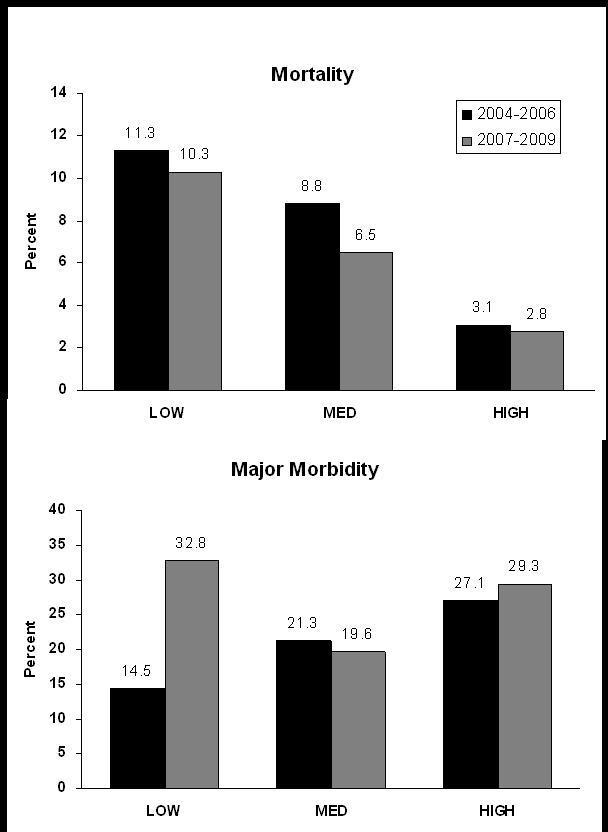
Introduction: Pancreaticoduodenectomy (PD) for pancreatic cancer carries a significant morbidity and mortality. Current evidence suggests that hospitals with a high annual PD volume provide improved outcomes after PD for cancer and regionalization to specialty centers is advocated. While better outcomes at high-volume centers (HVCs) are accepted, a rapid regionalization process could also have detrimental effects. For example, HVCs must be equipped to accommodate increased volume without compromising outcomes. North Carolina (NC) is unique in that there are multiple HVCs within the state to accommodate regionalization, including the establishment of our HVC in late 2006. Upon noting an increase in referral for surgical evaluation since 2007, we began investigation into regionalization of PD and its effects upon outcomes during this transition period within NC.Methods: The NC Hospital Based And Freestanding Ambulatory Surgery Facility Database was queried by ICD-9 code for all PD performed in NC during two time periods: 2004-06 and 2007-09. Hospitals were categorized by overall PD volume into three groups: Low (1-9 PD/yr), medium (10-19 PD/yr), and high (≥20 PD/yr) volume. Regionalization and operative mortality and major morbidity of PD performed for pancreatic cancer were assessed by comparing volume groups across time periods. Statistical analysis was performed using Chi-Square and Fisher’s Exact Test on SAS Software.Results: The number of PD for pancreatic cancer increased by 91% (129 to 246 cases) at HVCs while decreasing at low-volume (62 to 58 cases) and medium-volume (80 to 46 cases) centers. The percentage of PD for pancreatic cancer performed at HVCs increased significantly (47.6% to 70.3%), while decreasing for low- and medium-volume centers (p<0.001) (Fig 1). Mortality was significantly less at HVCs (2.8%) compared to low-volume centers (10.3%) for the 2007-09 timeframe (p=0.038), and was not different across periods for any group (Fig 2a). Mortality for all PD performed for pancreatic cancer in NC decreased from 6.6% to 4.6% across time periods (p=0.31). Major morbidity was not significantly different between volume groups within either time period; however, there was a significant increase in major morbidity at low-volume centers (p=0.018) (Fig 2b). Conclusions: Regionalization of PD for pancreatic cancer is occurring in NC, with a near doubling of PD performed at HVCs across these time periods. Mortality was significantly lower at HVCs during the most recent period, and importantly, this rapid and substantial regionalization has only served to enhance outcomes at HVCs. The very low mortality rate at HVCs despite a major morbidity rate comparable to low- and medium-volume centers is an intriguing finding that likely indicates higher case complexity with early complication recognition and management to “rescue” these patients.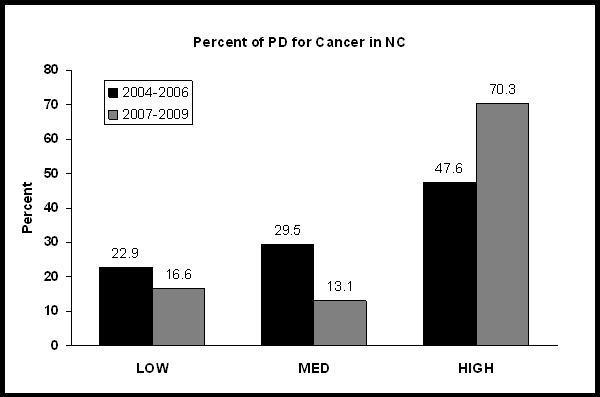
Back to 2011 Program



