Obesity Does Not Affect Outcomes in Gastro-Esophageal Cancer
Russell Farmer*, Kelly M. Mcmasters, Charles R. Scoggins, Robert C. Martin
Dept of Surgery, University of Louisville, Louisville, KY
BACKGROUND: Obesity is a growing epidemic in the United States. The CDC estimates that 25.6% of all adults in the US have a Body Mass Index (BMI) > 30. Obesity and its associated comorbidities have been shown to increase risk for perioperative complications. The purpose of this study was to compare the rate of complication in normal vs. obese patients undergoing esophageal anastomosis following oncologic resection. METHODS: We reviewed our prospective 350 patient esophageal-gastric database and found 166 esophageal anastomoses performed for esophageal and gastric cancer from 1994 to 2009, 157 with BMI data. With informed consent and IRB approval, we compared clinical, pathologic, and outcomes data in the perioperative period between patients with BMI ≥ 30 and BMI < 30. We then evaluated the presence of complication, severity of complication as indicated by the 5 point Clavien grading scale, and overall survival. Statistical correlations were calculated with Chi-Square (Monte-Carlo), independent T-test, Kaplan-Meier, and log-rank analyses as appropriate.RESULTS: Of the 157 patients reviewed with a median age of 62 (range 17 - 84);120 (76.4%) were men, 37 women, 40 were Obese (25.5%) and 117 were not Obese (74.5%). Of these 157 patients, 62 (39.4%) had neoadjuvant chemotherapy with 59 (37.5%) adjuvant treatment. No statistically significant difference was seen between the obese and non-obese patients regarding development of perioperative complication (72.5% vs. 62.4%, p = .268, 95% CI .198 - .377), grade of complication (p = .471, 95% CI .393 - .549), or anastomotic leak (25% vs. 20.5%, p = .745, 95% CI .687-.813). Intraoperative variables also showed no significant difference including: estimated blood loss (EBL) (p = .985), need for transfusion (P=.863), number of units transfused (p=.522), number of nodes collected on lymphadenectomy (p = .420). There was a decreased incidence of positive margin after resection in the Obese (2.5%) than non-Obese (12.0%) (p = .079, 95% CI = .075 - .180). In the superobese (BMI > 35), there was a significant trend toward greater intraoperative transfusion (4.5 vs. 2.4 units, p=.006) and increased mean number of positive lymph nodes on (8.9 vs. 3.9, p = .024). There was no difference in overall survival in the Obese with median of 16 months (range 0-180 months) and non-Obese 16.5 months (range = 0 - 180 months), (p=.968).CONCLUSIONS: Obesity does not affect rate of complication, grade of complication, or rate of anastomotic leak, or overall survival in patients undergoing esophageal anastomosis for oncologic resection. Further investigation is needed to determine the effect of obesity on margin positive resection as a function of procedure-limiting body habitus.
Clinical Outcomes After Esophagectomy Stratified by BMI > 30
| Normal BMIN = 117 | Obese (BMI > 30)N = 40 | P value | 95% Confidence Interval | Significant? | |
| Factor | |||||
| Leak | 24 (20.5%) | 10 (25%) | .745 | .677-.813 | No |
| Complication | 73 (62.4%) | 29 (72.5%) | .268 | .198-.377 | No |
| Clavien Complication Grade 3+ | 49 (41.9%) | 20 (50%) | .471 | .393-.549 | No |
| EBL: mean, (SEM) | 486.9 (43.1) | 485 (58.2) | .985 | (-)165 - (+) 168 | No |
| Transfusion given | 45 (38.5%) | 16 (40%) | 1.00 | .961-1.00 | No |
| Units transfused: mean, median (SEM) | 2.47, 2, (.18) | 2.75, 2, (.536) | .522 | -1.16 - .599 | No |
| Margin Positivity | 14 (12.0%) | 1 (2.5%) | .079 | .075 - .180 | No |
| Nodes removed: mean, (SEM) | 18.9 (1.26) | 20.9 (2.10) | .420 | -6.89 - 2.89 | No |
| Positive nodes: mean, (SEM) | 4.15 (.76) | 5.35 (1.51) | .449 | -4.30 - 1.91 | No |
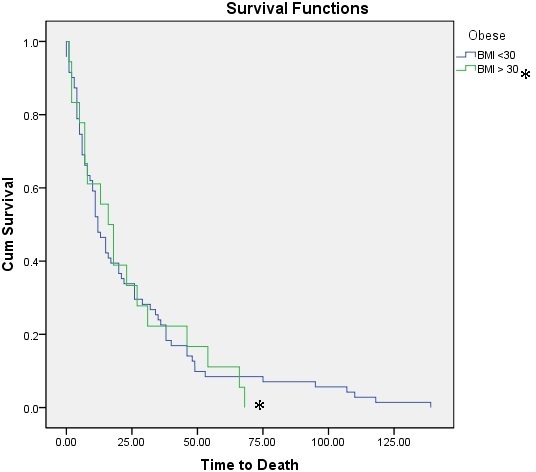
Overall Survival Following Esophageal Anastomosis: BMI < 30 vs. BMI > 30
Back to 2011 Program



