Back to Program | 2010 Program and Abstracts Overview | 2010 Posters
Safety and Efficacy of Curative Intent Surgery for Peri-Ampullary Liver Metastasis
Mechteld C. De Jong*, Susan Tsai, John L. Cameron, Barish H. Edil, Michael a. Choti, Richard D. Schulick, Christopher L. Wolfgang, Timothy M. Pawlik
Department of Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Surgery in the management of patients(pts) with peri-ampullary liver metastasis remains controversial. We assess safety and efficacy of curative intent surgery for peri-ampullary liver metastasis.Methods: Between 1993-2009, 40 pts underwent resection and/or radiofrequency ablation (RFA) for peri-ampullary liver metastasis. Clinicopathologic and outcome data were collected and analyzed.Results: Location of primary tumor was pancreatic head (n=20), ampullary (n=10), distal bile duct (n=5) or duodenum (n=5). Most pts (n=27) presented with synchronous disease. Of pts with metachronous diasease (n=13), median time to liver metastasis was 22mo. The majority of pts had solitary lesions (n=34); median lesion size was 2.7cm. Pts with simultaneous disease had smaller lesions (median, 0.9cm) vs pts with metachronous disease (median, 3.0cm)(p<0.01). At surgery, pts underwent resection alone (n=31), RFA alone (n=8), or resection+RFA (n=1). RFA alone (n=7, p<0.001) and resection ≥3 segments (n=5, p=0.009) were performed more often in pts with metachronous disease. Post-operative morbidity and mortality was 30% and 5% respectively. Most pts (55%) recurred with a median recurrence-free survival of 10mo. Intra-hepatic recurrence was the predominant pattern of initial recurrence (86%). Overall 1- and 3- year survival was 55% and 18%. Survival was not associated with synchronous vs metachronous presentation (p>0.05). Pts with pancreatic or distal bile duct tumors had a worse survival (median, 13mo) vs pts with ampullary or duodenal tumors (median, 23mo)(Fig 1).Conclusion: Surgery for peri-ampullary liver metastasis is associated with low morbidity and mortality. While survival is possible in select pts, outcome following surgery of peri-ampullary metastasis remains poor. Pts with ampullary or duodenal primaries benefit most from curative intent surgery.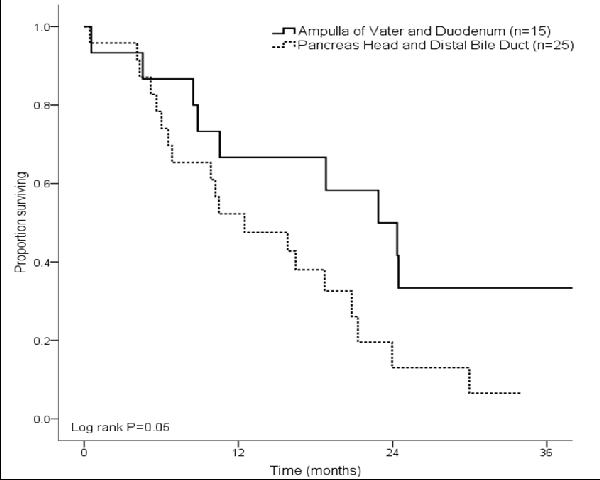
Back to Program | 2010 Program and Abstracts Overview | 2010 Posters



