WEIGHING THE OPTIONS: ATTITUDES AND PERCEPTIONS OF BARIATRIC SURGERY AMONGST PROVIDERS BASED ON REFERRAL PATTERNS
Lee Ying*2, Ysabel C. Ilagan-Ying1, Mariana Almeida3, Artur V. Viana1, Yihan Yang1, John Morton2, Albert Do1
1Internal Medicine, Yale University Department of Internal Medicine, New Haven, CT; 2Yale New Haven Health System, New Haven, CT; 3Yale University School of Medicine, New Haven, CT
Introduction: Bariatric surgery has emerged as one of the most effective treatments for obesity and its associated co-morbidities, but it is estimated that only 1% of patients eligible for bariatric surgery receive it. Previous studies have assessed the attitudes of referring providers towards bariatric surgery. In this study, we compare the characteristics and attitudes of providers who have increased their referrals for bariatric surgery compared to those who have not.
Methods: A 50-question electronic survey was conducted at a large, tertiary academic center from May through October 2020. Referring providers of all training levels (residents, fellows, and attendings) were surveyed on their demographics, perceptions of bariatric surgery, and practices patterns. Frequency and univariate analyses were performed and compared provider demographics, practice patterns, and perceptions of bariatric surgery between those who reported increased rates of referrals for bariatric surgery compared to those who did not.
Results: There were 131 complete survey responses out of the 779 physicians surveyed (16.8% response rate). Providers were stratified by self-reported increase rate in bariatric surgery referrals in the antecedent year (n=49) compared to not increased (n=82). (Table 1) Respondents reporting increased referrals were more likely to be older (39.1 vs. 36.1 years, p=0.012), have spent more time in training (6.6 vs. 4.6 years, p=0.002), and to have received information about bariatric surgery within the past year (30.6% vs 16.5%, p=0.048). They also reported higher comfort with explaining sleeve gastrectomy (2.3 vs. 1.6 on a 6-point Likert scale, p=0.006) and gastric bypass (2.4 vs. 1.7, p=0.008), and were more willing to refer themselves or family (85.7% vs. 67.9%, p=0.022). Those with increased referrals perceived surgery to be more effective for weight loss (3.9 vs. 3.5, p=0.024) (Figure 1A). There were no significant differences in knowledge of surgical mortality rate between the two groups, but providers who did not increase their referrals were more likely to believe that surgery and medical weight loss programs were equally effective (Figure 1B).
Discussion: We report for the first time a comparison of the attitudes and perceptions of providers across multiple training levels and disciplines at the same tertiary academic institution who have or have not increased their referrals to bariatric surgery. Those with increased rates of referrals for bariatric surgery reported receiving more information and greater comfort in explaining these interventions, and were more willing to refer themselves or family for bariatric surgery.
Conclusion: Promoting education about the techniques and mechanisms of bariatric surgery, as well as highlighting differences in outcomes between surgical weight loss and medical weight loss may improve patient access.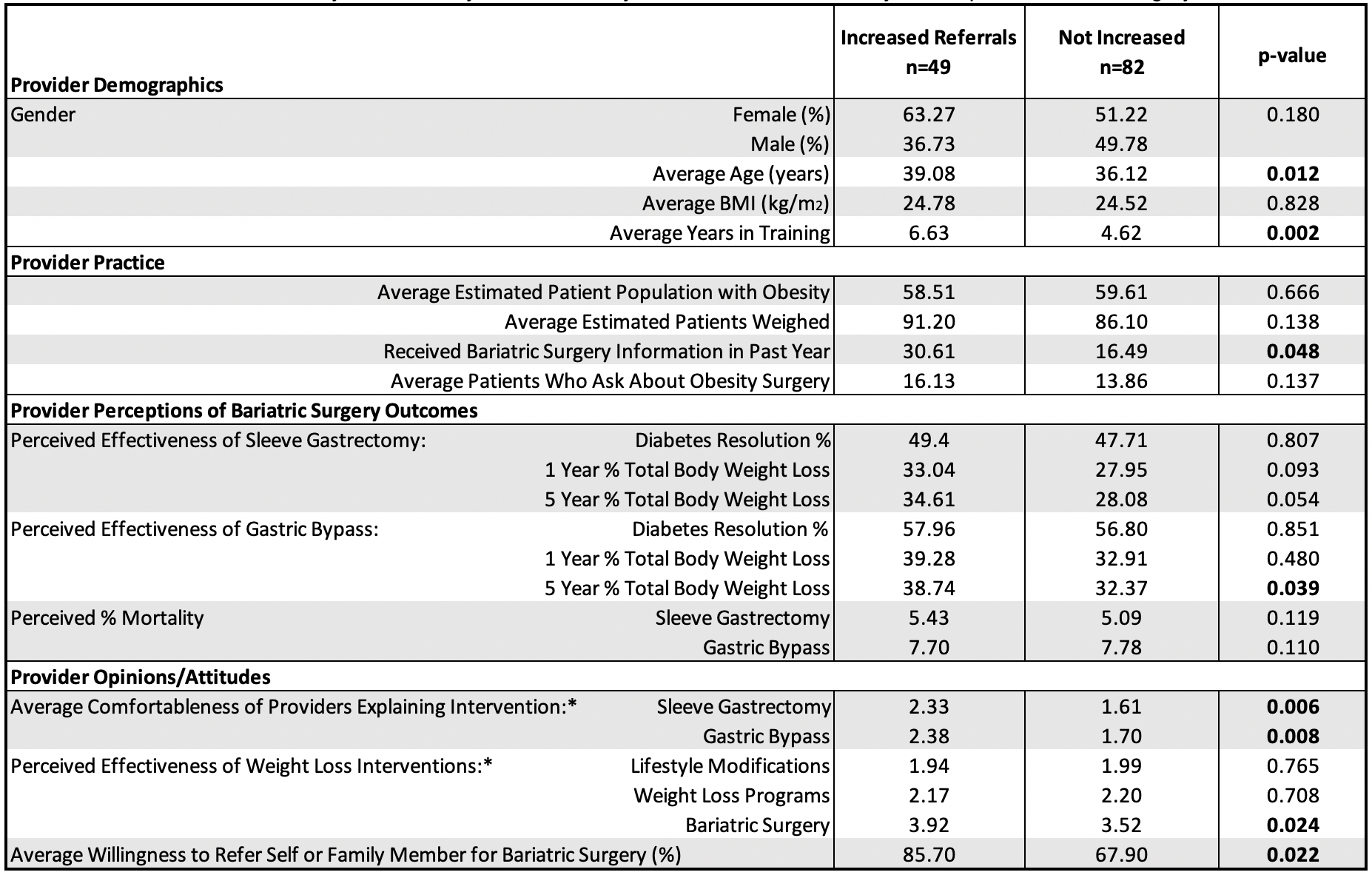
Table 1. Characteristics of 131 Physicians Surveyed Between May-October 2020, Stratified By Self-Reported Bariatric Surgery Referral Patterns. *Likert Scale Rating (1=Not at all, 2=Mildly, 3=Somewhat, 4=Quite, 5=Mostly, 6=Very); Univariate statistics were performed as follows: categorial data using a chi-square tests, ordinal data (Likert scale) using Mann-Whitney-U tests, and continuous data using t-tests.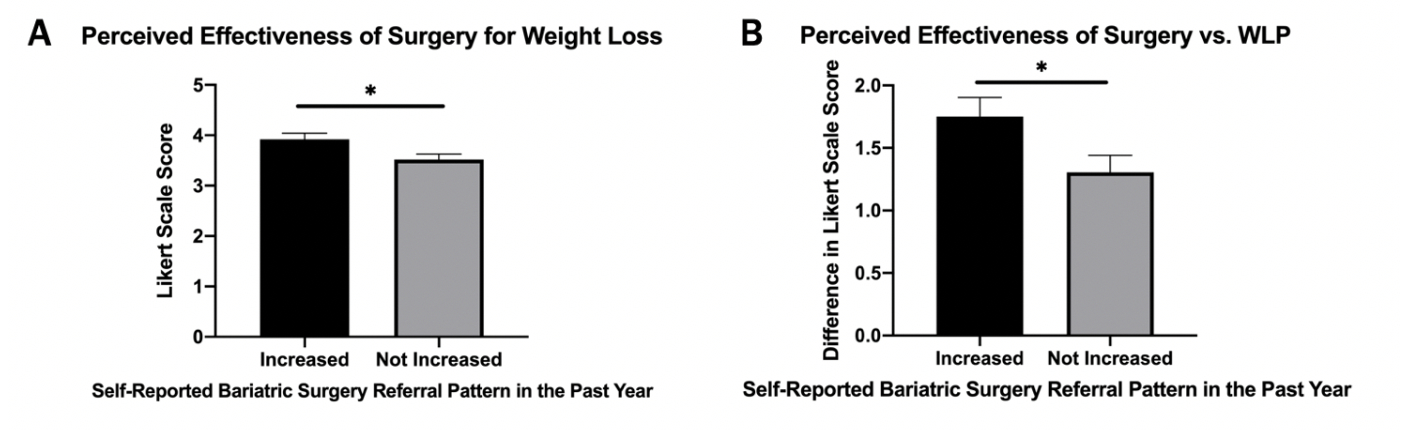
Figure 1. Perceptions of Bariatric Surgery. A) Physicians who did not report increased rates of referrals for bariatric surgery in the past year had lower perceptions of effectiveness of surgery for weight loss compared to those with increased referrals. B) Physicians who reported increased rates of referrals for bariatric surgery in the past year perceived a greater difference in effectiveness of bariatric surgery compared to weight loss programs (WLP). *p<0.05
Back to 2021 Abstracts
