SURGICAL TREATMENT OF RADIOINDUCED ESOPHAGEAL CANCER: RESULTS OF A SINGLE CENTER CASE-CONTROL STUDY WITH PROPENSITY SCORE MATCHING
Giovanni Capovilla*, Anna Laura De Pasqual, Elisa Sefora Pierobon, Lucia Moletta, Renato Salvador, Mario Costantini, Gianpietro Zanchettin, Luca Provenzano, Stefano Merigliano, Michele Valmasoni
University of Padova, Padova, Italy
Background: The clinical behavior, treatment strategies and prognosis of radiotherapy-induced esophageal cancer (RIEC) remains poorly defined. In particular, there is no consensus about the feasibility of neoadjuvant chemoradiotherapy (nCRT) for the treatment of a cancer occurring in a previously irradiated field. The aim of our study was to evaluate the outcome of surgery for RIEC, by comparing the postoperative outcome of patients who underwent surgery with and without nCRT for RIEC with a matched control group of patients treated for primary non-radioinduced esophageal cancer (PEC).
Methods: All patients who underwent esophagectomy for PEC or RIEC with a curative intent at our Department between 1981 and 2020 were analyzed. Only patients meeting Cahan's criteria for defining EC as radioinduced were deemed available for evaluation. Two groups of surgically treated patients were generated by propensity score matching: a case group of patients with RIEC (RIEC group) and a control group of patients with PEC (PEC group).
Results: During the study period 5552 patients affected by PEC and 94 affected by RIEC were observed. As a result of the matching process, 50 patients with PEC (PEC group) and 51 patients with RIEC (RIEC group) were compared. Demographic and clinical characteristics of the two groups are reported in Table 1. Overall, there were no significant differences between the RIEC group and the PEC group. The nCRT was administered to the RIEC group and the PEC group in similar proportions (43% vs 50%; p=0.49), with no differences in the response rate between the groups according to the RECIST criteria (p=0.73). Treatment outcomes are reported in Table 2. Overall, there were no differences in the surgical outcome between the two groups. The incidence of postoperative complications was also not significantly different (p=0.09) however the incidence of Clavien-Dindo > 3 complications was significantly higher in the RIEC group (p=0.04). There were no differences in disease free survival (DFS) (p=0.38) and overall survival (OS) (p=0.20) between RIEC and PEC.
Conclusions: In contrast with other studies, short and long-term outcomes of patients with RIEC were comparable to patients with PEC. The incidence of postoperative complications was similar between the two groups, however, their severity was significantly higher in the RIEC group. A previous history of radiation should not be considered as a contraindication to nCRT or radical surgery in this highly selected and challenging subset of patients.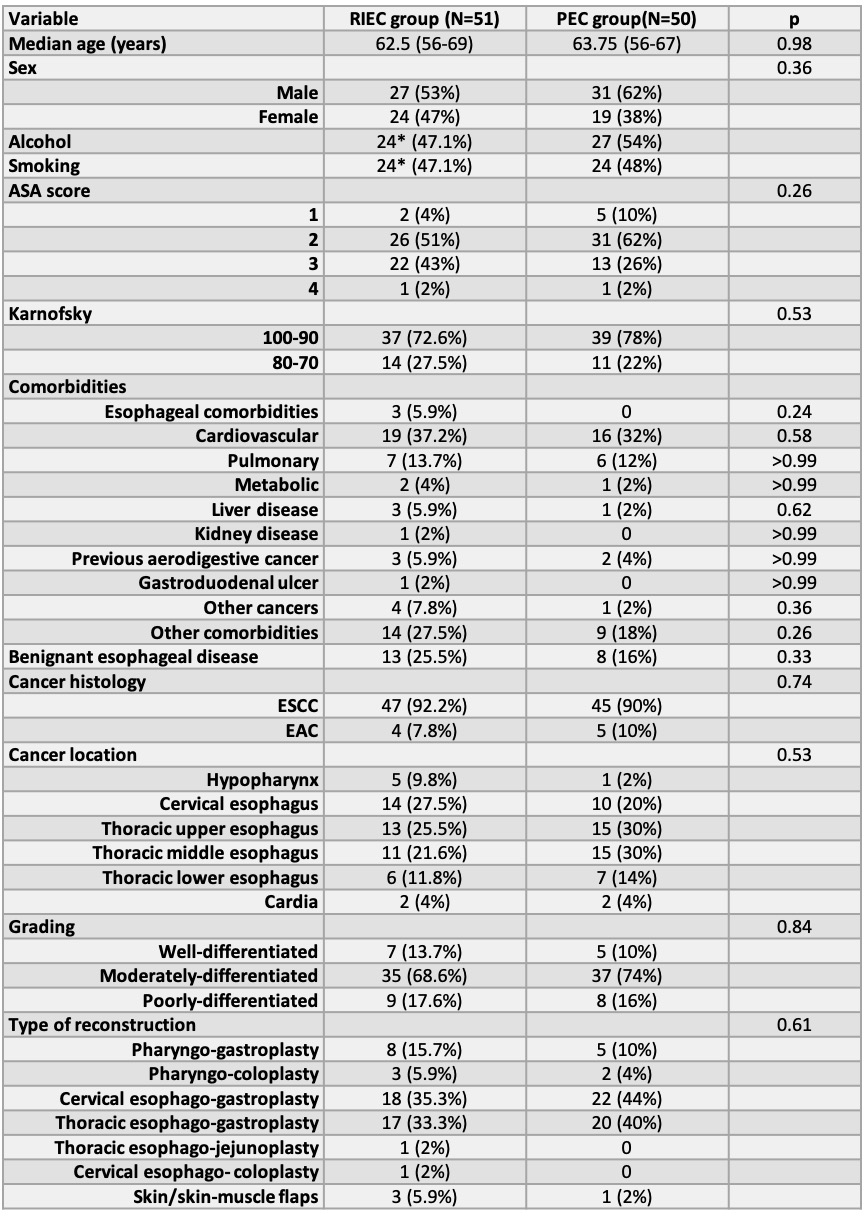
Table 1: Demographic and clinical characteristics of RIEC group and PEC group
*Data available for 46 patients.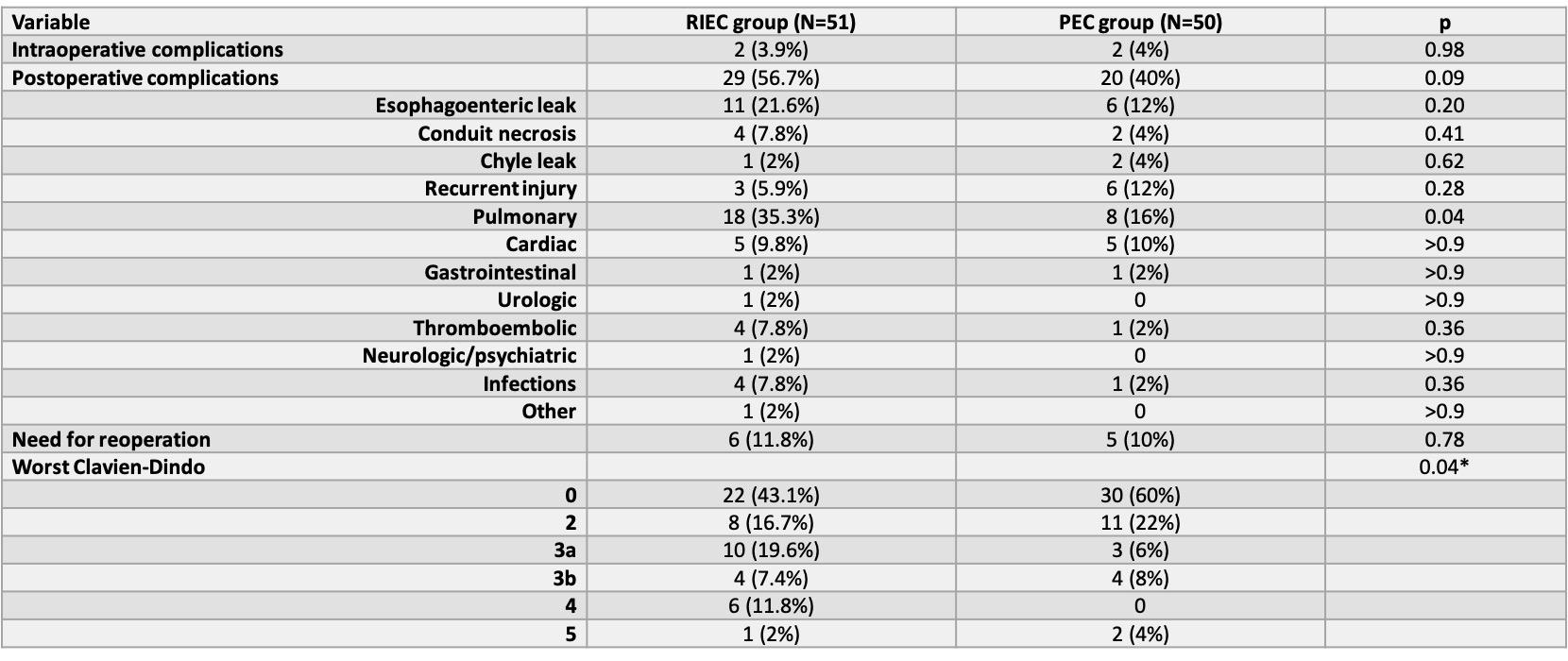
Table 2: Treatment outcomes.
*chi square test for trend
Back to 2021 Abstracts
