REDUCED WRAP DISTENSIBILITY PREDICTS DYSPHAGIA AMONG PATIENTS WITH PARTIAL, BUT NOT COMPLETE, FUNDOPLICATION
Lester Tsai*, Santiago Horgan, Bryan J. Sandler, Ryan C. Broderick, Alice J. Race, David C. Kunkel
Internal Medicine, University of California San Diego, San Diego, CA
INTRODUCTION
Multiple studies have demonstrated decreased esophagogastric junction (EGJ) distensibility immediately following fundoplication, with complete wraps generally lower than partial ones. What remains unclear is the post-operative relationship between EGJ-wrap distensibility and development of esophageal symptoms such as dysphagia. If distensibility index (DI) is to be used as an objective parameter for decisions regarding downstream interventions, then ideally it should correlate with a patient's esophageal symptoms. We set out to investigate how EGJ-wrap distensibility varies by type of fundoplication and by presence of dysphagia.
METHODS
We performed a retrospective chart review of 37 consecutive patients with fundoplication who underwent EndoFLIP procedures between June 2017 and September 2020. Baseline characteristics including demographics, relevant medical history, and type of fundoplication were recorded. Data collected from EndoFLIP procedures included balloon catheter used, indication, and EGJ-wrap DI at fill volumes of 30, 40, 50 and 60 mL. Patients were divided into 6 groups based on fundoplication subtype (Toupet, Dor, Nissen) and indication (dysphagia versus no dysphagia).
RESULTS
There were 42 EndoFLIP procedures (62% with EF-325, 38% with EF-322) performed in 37 patients with Toupet (n = 9), Dor (n = 8), and Nissen (n = 25) wraps. When comparing the mean EGJ-wrap DI at the 40mL fill volume, there were significant differences between patients with dysphagia and no dysphagia in the Toupet cohort (1.2 '± 0.6 versus 5.2 '± 2.5, p = .003) and Dor cohort (3.7 '± 2.6 versus 10.4 '± 1.6, p = .016), but not in the Nissen cohort (3.0 '± 2.2 versus 2.6 '± 1.7; p = .739). When comparing the mean EGJ-wrap DI across all fill volumes, there were significant differences between patients with dysphagia and no dysphagia in the Toupet cohort (1.6 '± 1.4 versus 5.0 '± 2.2, p = .0005) and Dor cohort (3.7 '± 2.4 versus 10.0 '± 0.9, p = .0001), but not in the Nissen cohort (3.0 '± 1.9 versus 3.2 '± 2.2, p = .66).
DISCUSSION
In this study, EGJ-wrap DI reliably predicted dysphagia in patients with partial fundoplication. In particular, distensibility was reduced in patients experiencing dysphagia, consistent with a tighter wrap, and significantly higher in those experiencing symptoms without dysphagia, consistent with a looser wrap. These differences were seen across multiple fill volumes in patients with either a Toupet or Dor fundoplication. In contrast, no such relationship was seen in patients with Nissen fundoplication, which suggests that the underlying etiology is multifactorial and that problems may exist beyond the EGJ-wrap, for example involving esophageal motility. Altogether, these findings highlight the prognostic value of EndoFLIP distensibility testing in patients with partial wraps, which can subsequently guide therapeutic management.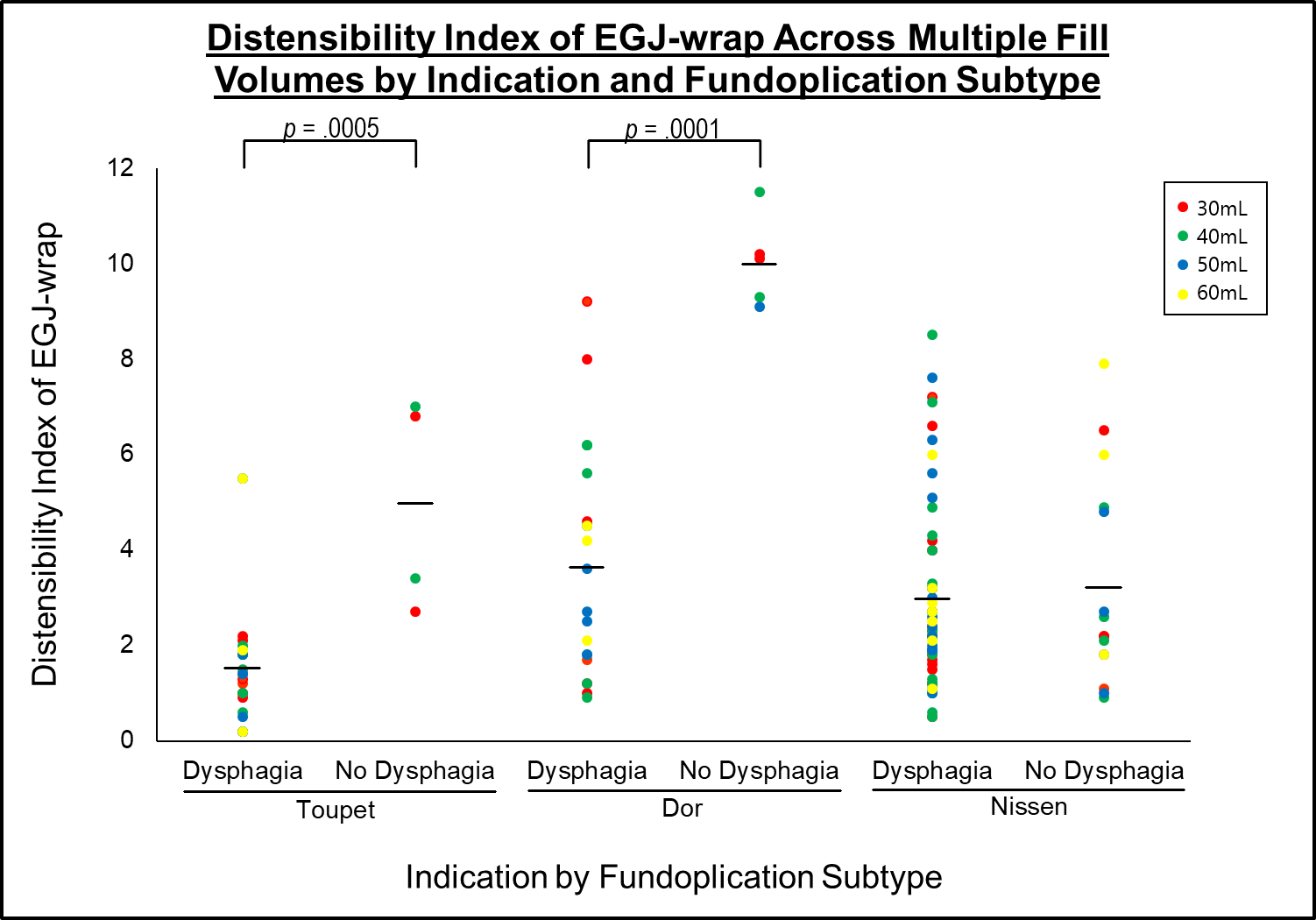
Back to 2021 Abstracts
