IMPACT OF ENHANCED RECOVERY PATHWAY (ERP) ON SURGICAL DISPARITIES FOR PATIENTS WITH INFLAMMATORY BOWEL DISEASE
Lauren Theiss*, Tara Wood, Connie Shao, Isabel Marques, Robert H. Hollis, Drew J. Gunnells, Karin M. Hardiman, Jamie A. Cannon, Gregory D. Kennedy, Melanie S. Morris, Daniel I. Chu
University of Alabama at Birmingham (UAB), Birmingham, AL
Introduction:
Racial disparities in surgical outcomes exist. Previous studies have demonstrated that enhanced recovery pathways (ERP) may reduce racial disparities in length of stay (LOS) after colorectal surgery. However, it is unknown whether ERP may similarly mitigate surgical disparities among patients with inflammatory bowel disease (IBD). We hypothesized that implementation of ERP would reduce disparities in postoperative outcomes experienced by Black patients with IBD.
Methods:
Patients undergoing elective inpatient abdominal surgery for IBD at a tertiary care referral center between 2006-2020 were enrolled in the study. An ERP was implemented in December 2014. Patients were stratified into 2 groups: pre-ERP and ERP. The American College of Surgeons National Surgical Quality Improvement Program database was queried for patient characteristics as well as postoperative LOS, 30 day readmissions, complications, and mortality. Outcomes were compared overall between pre-ERP and ERP cohorts, between Black and white patients in the pre-ERP cohort, and Black and white patients in the ERP cohort. Bivariate comparisons were performed with alpha of 0.05 set a priori.
Results:
Overall, 454 patients with IBD were included in the study. 298 patients underwent surgery pre-ERP and 156 underwent surgery under ERP. Overall, mean age was 42.1 years (SD 15.2), 46.0% of patients were female, 16.1% of patients were Black and 83.3% were white. Patients undergoing surgery under ERP were more likely to have Crohn's Disease (62.2% vs. 49.5%, p=0.01) but were less likely to be on steroids preoperatively (32.1% vs. 45.6%, p=0.005). There were no other significant differences in patient characteristics between pre-ERP and ERP groups. Overall, ERP patients experienced a median LOS of 4 days vs. 6 days in pre-ERP group (p<0.001). There were no significant differences in readmissions, complications or mortality overall between pre-ERP and ERP groups.
In the pre-ERP group, racial disparities in LOS existed with median LOS of 7 days for Black patients vs. 6 days for white patients (p=0.02). Black patients also experienced disparities in complications, with 40.9% Black patients experiencing a complication vs. 25.9% white patients (p=0.041). Under ERP, racial disparities in LOS were mitigated with median LOS of 4 days for both Black and white patients (Figure 1). However, the disparity in complications persisted and a disparity in rates of readmission widened under ERP (31.0% readmission for Black patients vs. 12.6% white, p=0.015, Figure 2).
Conclusion:
Racial disparities exist among patients undergoing surgery for IBD. ERP improves LOS for all patients and may mitigate disparities in LOS. However, Black patients with IBD may experience disparities in readmission and complications even under ERP. Thus, further interventions are required to eliminate surgical disparities.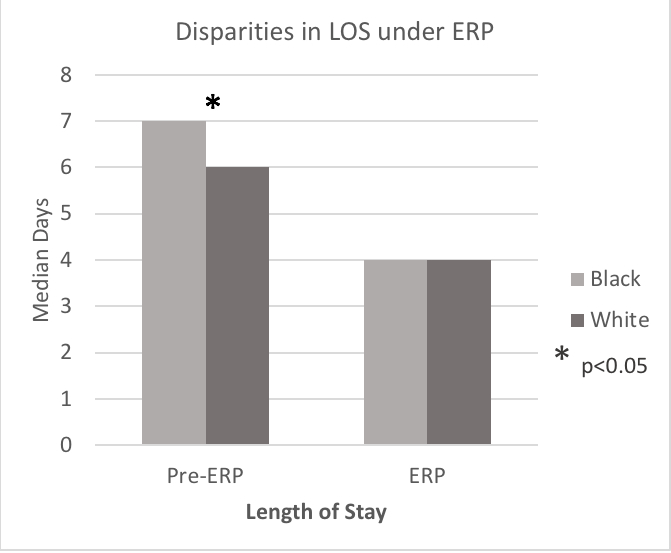
Figure 1. Disparities in LOS under ERP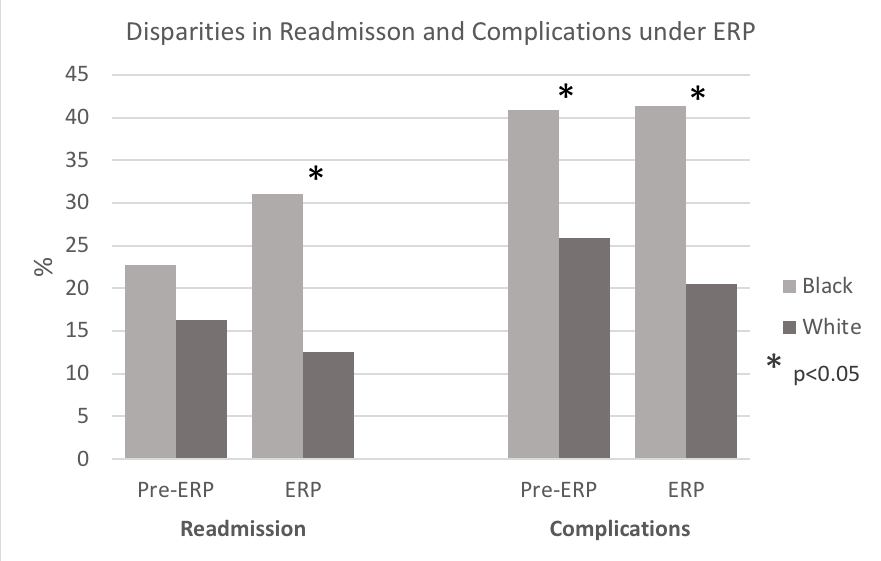
Figure 2. Disparities in Readmisson and Complications under ERP
Back to 2021 Abstracts
