IMPACT OF INFLAMMATORY BOWEL DISEASE ON RISK OF VENOUS THROMBOEMBOLISM IN PATIENTS UNDERGOING COLORECTAL CANCER SURGERY - A NATIONWIDE COHORT STUDY
Gencer Kurt*, Katalin Veres, Frederikke Schønfeldt Troelsen, Erzsébet Horváth-Puhó, Henrik Toft Sørensen, Rune Erichsen
Department of Clinical Epidemiology, Aarhus Universitetshospital, Aarhus N, Denmark
Background: Inflammatory bowel disease (IBD) is associated with increased mortality in patients undergoing colorectal cancer (CRC) surgery. Venous thromboembolism (VTE) is a serious complication following surgery that may represent an important intermediate in this association. We therefore investigated risk of VTE in patients with and without IBD undergoing first-time CRC surgery.
Methods: We conducted a nationwide population-based cohort study using data from Danish health and administrative registries (1996-2013). We included all patients undergoing first-time CRC surgery in Denmark from 1996-2012 to allow for at least one year of follow-up period. Patients with an IBD diagnosis prior to or on the date of CRC surgery were defined as exposed. We followed each patient from CRC surgery date until first occurrence of VTE (pulmonary embolism or deep venous thrombosis), death, emigration, or end of follow-up. We calculated 0-30-day and 0-365-day cumulative risk of VTE with death as competing risk. Cox proportional hazards regression was used to calculate hazard ratios (HRs) with 95% confidence intervals (CIs) associating IBD with VTE in patients undergoing CRC surgery. In the regression analyses, HRs were adjusted for sex, age group, year of CRC surgery, CRC location, CRC stage at diagnosis, and Charlson Comorbidity Index score.
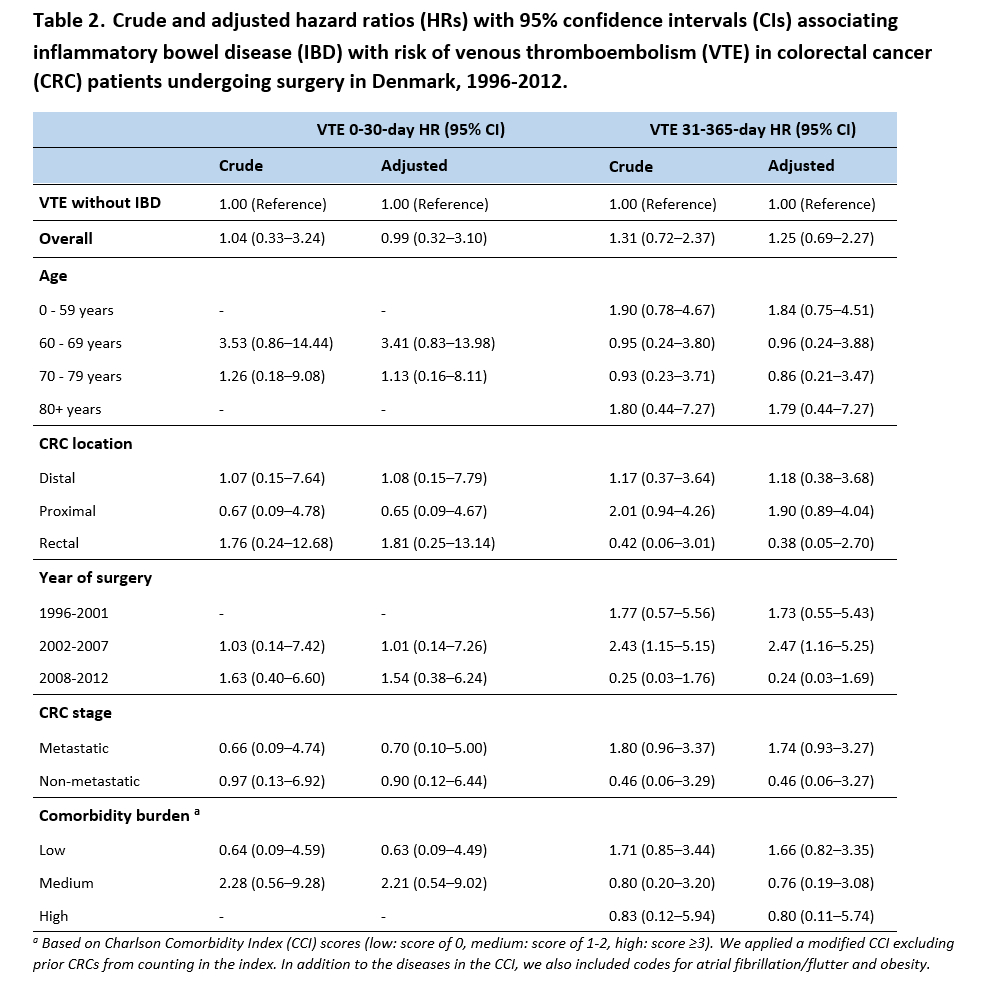
Results: We identified 52,779 patients undergoing first-time CRC surgery. Of these, 638 had IBD. Among patients with IBD, 14 were diagnosed with VTE during follow-up. The corresponding number was 915 in CRC patients without IBD. In IBD patients, the 0-30-day VTE risk after CRC surgery was 0.47% (95% CI: 0.13-1.30) and the 0-365-day risk was 2.19% (95% CI: 1.26-3.56). In patients without IBD, 0.46% (95% CI: 0.40-0.52) and 1.75% (95% CI: 1.64-1.87) experienced a VTE 0-30 days and 0-365 days after surgery, respectively. We observed a 0-30-day adjusted HR of 0.99 (95% CI: 0.32-3.10) and a 31-365-day adjusted HR of 1.25 (95% CI: 0.69-2.27).
Conclusion: CRC patients with and without IBD had similar risk of developing VTE within 30 days after CRC surgery. The risk of VTE 31-365 days after CRC surgery was slightly elevated in IBD patients compared with those without IBD. However, the estimates were imprecise and our findings require confirmation in larger studies.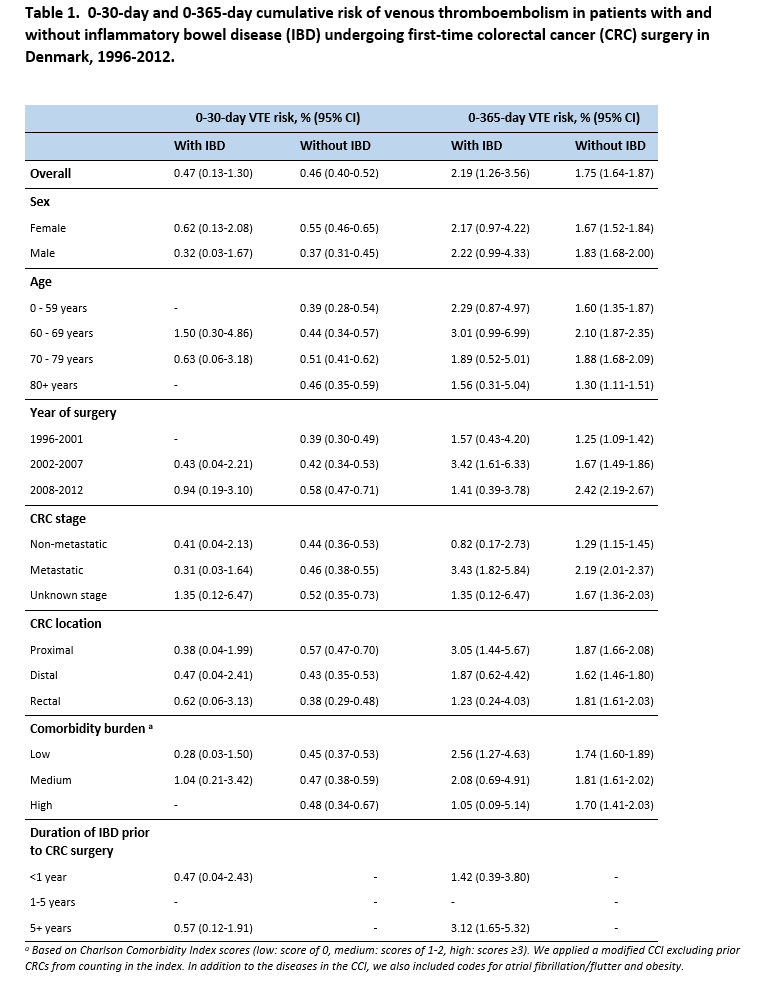
Back to 2021 Abstracts
