EARLY VERSUS LATE RECURRENCE IN RECTAL CANCER: DOES TIMING MATTER?
Marina Affi Koprowski*, Thomas L. Sutton, Nima Nabavizadeh, Charles R. Thomas, Emerson Chen, Adel Kardosh, Charles Lopez, Skye C. Mayo, Kim C. Lu, Daniel O. Herzig, Vassiliki L. Tsikitis
Oregon Health and Science University, Portland, OR
Background: Published data on the definition of early recurrence (ER) in rectal cancer are conflicting, though most use a 24-month cutoff. Additionally, the association of ER with post-recurrence survival (PRS) is poorly described. We therefore sought to identify if time to recurrence is associated with PRS.
Methods: We reviewed all curative-intent resections of nonmetastatic rectal cancer between 2003-2018 from our institutional cancer registry. Clinicopathologic data at diagnosis and recurrence were collected and analyzed. ER was pre-specified at <24 months post-resection and late recurrence (LR) at 24+ months. PRS was evaluated by the Kaplan-Meier method and Cox proportional-hazards modeling. To further evaluate the significance of time to recurrence, it was analyzed both as a continuous variable and with separate cutoffs of 12, 24, and 36 months.
Results: There were 548 patients who underwent resection for nonmetastatic rectal cancer during the study period; 61 patients recurred with a median time to death or last follow-up of 53 months (interquartile range (IQR) 30-89 months). Median time to recurrence was 14 months (IQR 10-18 months), and 45 patients (74%) had ER. There were no significant baseline clinicopathologic or pre-recurrence treatment differences between patients with ER and LR (all P>0.05), including receipt of radiation or systemic therapy. About half (n=32; 52%) of all patients received neoadjuvant chemoradiation. Nearly two-thirds (n=35; 57%) of recurrences were isolated to the liver (n=16; 26%) or lung (n=19; 31%), and 16% (n=10) were locoregional. Symptoms of recurrence prompting an evaluation were present in only 15% (n=9) of patients.
On Kaplan-Meier analysis, ER was not associated with worse PRS compared to LR (P=0.998, Figure 1). ER was also not associated with PRS when analyzed using the additional discrete cutoffs or when analyzed as a continuous variable (all P>0.2). On Cox multivariable analysis, the following were independently associated with PRS: detection of recurrence via workup for symptoms, CEA >10 ng/mL at recurrence, and site of recurrence (Table 1).
Conclusion: ER, regardless of its definition, is not associated with PRS in patients with resected rectal cancer. Symptomatic recurrences of rectal cancer and those accompanied by CEA elevations are associated with worse PRS, while metastatic disease confined to the liver or lung is associated with improved PRS. "Early recurrence" should not be viewed as an independent prognosticator of survival. Instead, attention should be directed toward counseling patients with symptoms at recurrence and determining appropriate surgical, radiation, and systemic therapies for patients with oligometastatic disease.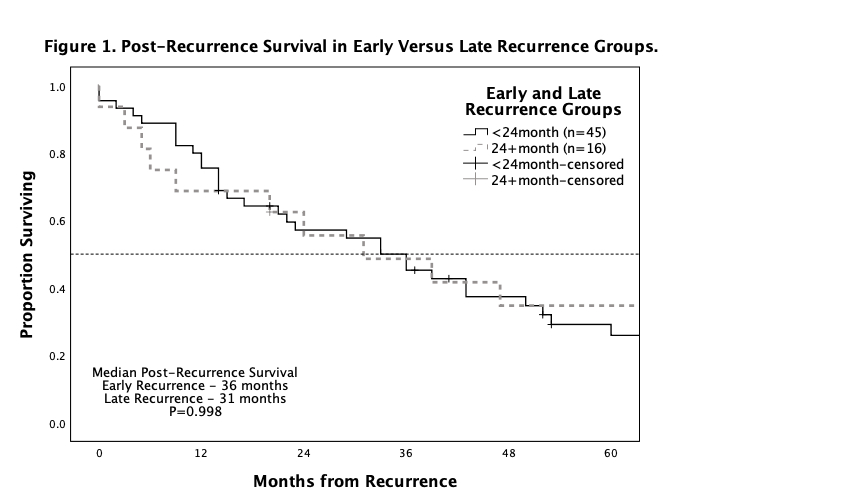
Kaplan-Meier curve demonstrating estimated median post-recurrence survival in early recurrence and late recurrence cohorts (36 and 31 months, respectively). There was no significant difference between the two groups (P=0.998).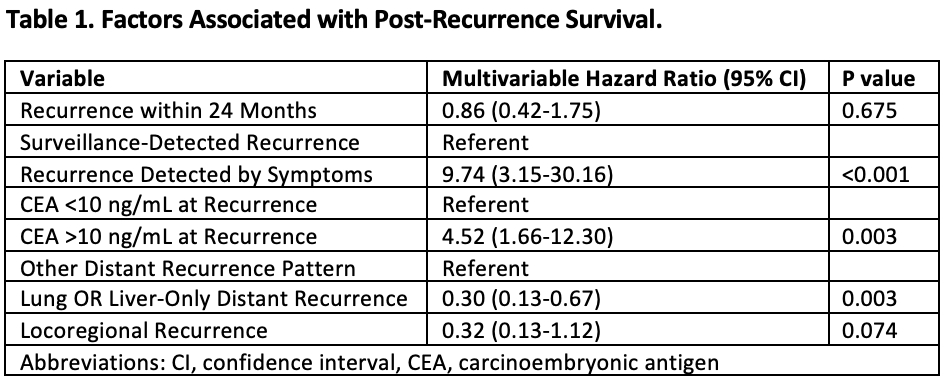
Multivariable analysis via Cox proportional-hazards model assessing factors associated with post-recurrence survival. Recurrence within 24 months was not associated with post-recurrence survival; however, recurrence detected via workup for symptoms, CEA >10 ng/mL at recurrence, and recurrence isolated to the liver or lung were all significantly associated with post-recurrence survival (all P<0.003).
Back to 2021 Abstracts
