EARLY VERSUS DELAYED CHOLECYSTECTOMY IN PATIENTS WITH ACUTE BILIARY PANCREATITIS A META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS
Hasan Shoaib*, Muhammad N. Asghar, Saqib Walayat, Sonu Dhillon, Steven S. Tsoraides
Internal Medicine, University of Illinois College of Medicine at Peoria, Peoria, IL
Background
Since 1985, when the first laparoscopic cholecystectomy was performed, there has been an ongoing debate whether early cholecystectomy in acute biliary pancreatitis has better outcomes compared to the conventional approach of undergoing a delayed one. 1 Recent studies have shown early cholecystectomy to have improved outcomes with decreased biliary complications. 2
Aims
This meta-analysis of randomized controlled trials was performed to compare the outcomes of patients with acute biliary pancreatitis undergoing early cholecystectomy versus delayed cholecystectomy. The primary outcome is complications while the secondary outcomes include intra-operative complications, post-operative complications, and the rate of conversion of laparoscopic cholecystectomy to open cholecystectomy.
Methods
Review Manager 5.4 was used to analyze the data in this meta-analysis. Only randomized controlled trials, comparing early versus delayed cholecystectomy in patient's with acute biliary pancreatitis, were included in this meta-analysis and databases were searched from January 1992 to October 2020. These databases included but not limited to Medline, Ovid, PubMed and Cochrane. The outcomes that were analyzed were biliary complications, intra-operative complications, post-operative complications, and conversion of laparoscopic cholecystectomy to open cholecystectomy.
Results
A total of 10 randomized controlled trails were included in our study that encompassed 1,118 patients. Biliary complications were significantly less in patient's that underwent early cholecystectomy with an odds ratio of 0.16 CI 0.09 - 0.27 P < 0.00001 compared to the delayed group Figure 1. Heterogeneity for this subgroup analysis was insignificant Heterogeneity: Chi square = 12.65, df = 8 P = 0.12 I square = 37%. However, the secondary outcomes which included intra-operative complications OR 0.57, CI 0.17 - 1.84, P = 0.34, post-operative complications OR 0.74, CI 0.43 - 1.30, P = 0.30 and conversions OR 1.19, CI 0.63 - 2.24, P = 0.59 were not significant between the two groups.
Conclusion
This study showed a significant decrease in biliary complications if the laparoscopic cholecystectomy was performed earlier in the disease process of acute biliary pancreatitis compared to the latter. Further meta-analysis and randomized controlled trials, with a stringent criterion that defines early cholecystectomy, could potentially show the perfect time period within which the procedure should be performed to reduce complications.
1. Reynolds Jr W. The first laparoscopic cholecystectomy. JSLS: Journal of the Society of Laparoendoscopic Surgeons. 2001 Jan 5 1:89.
2. Mueck KM, Wei S, Pedroza C, Bernardi K, Jackson ML, Liang MK, Ko TC, Tyson JE, Kao LS. Gallstone Pancreatitis: Admission versus Normal Cholecystectomy-a Randomized Trial Gallstone PANC Trial. Annals of surgery. 2019 Sep 270 3:519.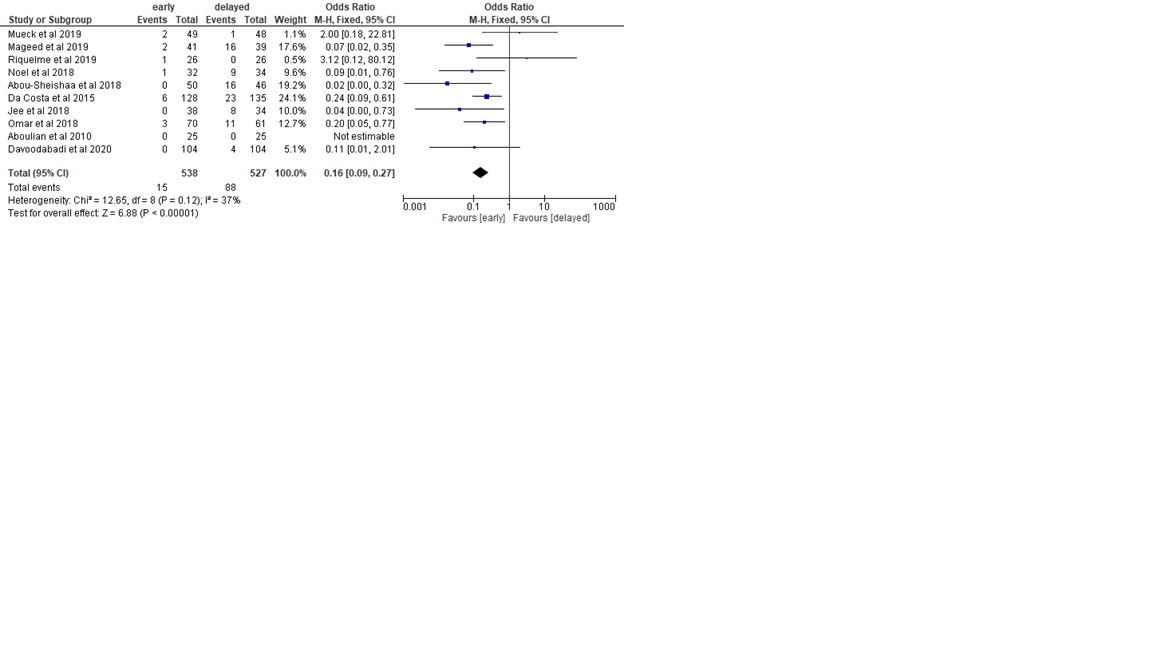
Back to 2021 Abstracts
