UTILIZATION OF THE KAWAGUCHI-GAYET COMPLEXITY CLASSIFICATION TO CREATE, IMPLEMENT, AND VALIDATE RISK-STRATIFIED POST-HEPATECTOMY PATHWAYS BASED ON ANTICIPATED LENGTH OF STAY
Bradford J. Kim*, Elsa M. Arvide, Yoshikuni Kawaguchi, Whitney L. Dewhurst, Teresa L. Phan, Hop Tran Cao, Thomas Aloia, Yun Shin Chun, Matthew Katz, Jean-Nicolas Vauthey, Ching-Wei D. Tzeng, Timothy E. Newhook
Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX
Background: The modified Kawaguchi-Gayet (K-G) classification is a validated system to stratify open liver resections by intraoperative complexity and postoperative complications. We hypothesized that the modified K-G classification could be used to create and implement distinct risk-stratified post-hepatectomy pathways (RSPHPs) aimed at reducing length of stay (LOS) and variation in care.
Methods: Clinicopathologic data from consecutive hepatectomy patients (1/2017-6/2020) were abstracted from a prospectively maintained quality improvement database, which tracked 90-day outcomes by ACCORDION grade (postoperative major complications, PMCs, defined as Grade '‰¥3). All hepatectomies were assigned to groups based on 2 levels of the K-G classification: Low-Intermediate (open K-G I/II) and High (open K-G III) risk. All combination (e.g. with colectomy, etc.) and minimally invasive hepatectomies were excluded. RSPHPs were formulated with a goal of reducing LOS by one day without increase in readmissions. LOS was compared between "PRE" (1/1/2017-9/30/2019) and "POST" (10/1/2019-6/30/2020) pathway periods.
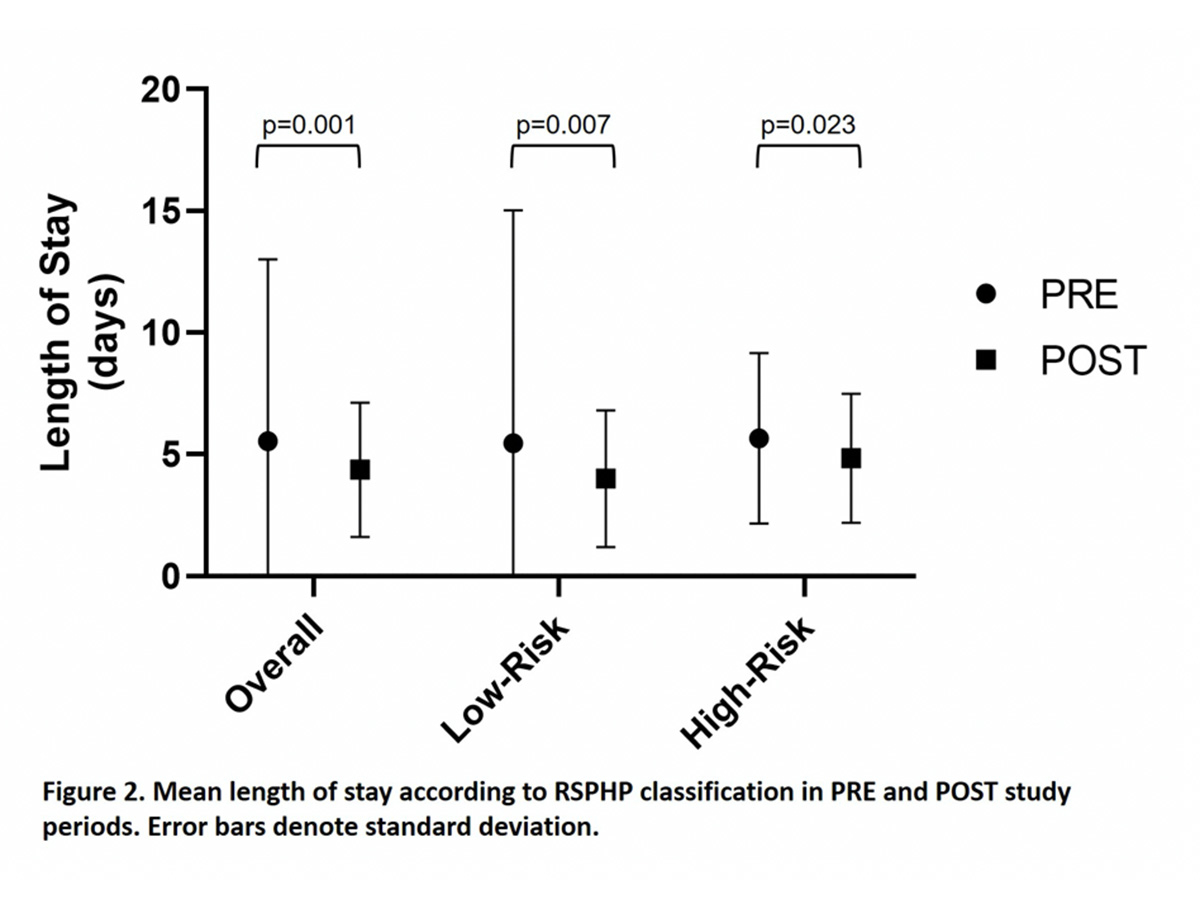
Results: Among the 487 included hepatectomies (PRE: 374, POST: 113), 55.0% (n=268) were Low-Intermediate and 45.0% (n=219) were High risk. PMC rates were similar within Low-Intermediate (PRE: 7.3%, POST: 7.9%, p=0.870) and High (PRE: 18.9%, POST 10.0%, p=0.139) categories. Before pathway implementation, LOS showed no annual improvement within the PRE period (Figure 1). Despite similar surgical outcomes between eras, implementation of RSPHPs reduced median LOS by one day for both Low-Intermediate (4 to 3 days, p=0.007) and High (5 to 4 days, p=0.023) risk patients. RSPHPs decreased variation in LOS as demonstrated by reduction in mean LOS and standard deviation (SD) for overall (PRE 5.5 '± 7.5 vs. POST 4.4 '± 2.8 days), Low-Intermediate (PRE 5.5 '± 9.6 vs. POST 4.0 '± 2.8 days), and High risk patients (PRE 5.7 '± 3.5 vs. 4.8 '± 2.7 days; Figure 2). There was no difference in 90-day readmission rates between PRE and POST periods (overall: 12.5% vs. 8.8%, Low-Intermediate: 7.8% vs. 4.8%, High: 18.3% vs. 14.0%; all p>0.05).
Conclusions: The K-G complexity classification was used to create and implement RSPHPs that were preoperatively assigned to hepatectomy patients, which was validated in the post-implementation period with reduced central tendency and variance in LOS. These no-cost generalizable RSPHPs grouped patients a priori into pathways for a more specific and individualized preoperative discussion on postoperative expectations and yielded improved hospital inpatient metrics.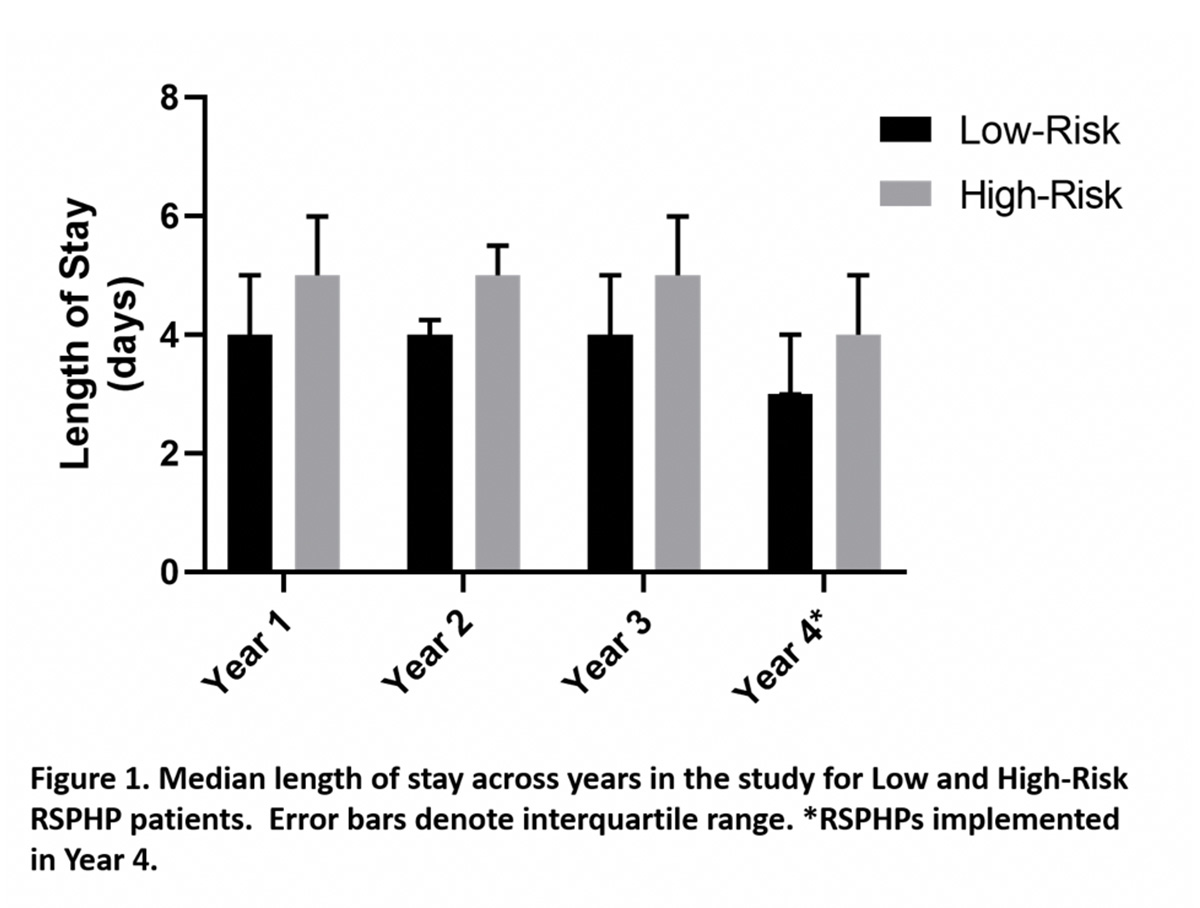
Back to 2021 Abstracts
