CARING FOR PATIENTS WITH COMPLICATIONS AFTER COMPLEX GASTROINTESTINAL SURGERY: A NATIONAL STUDY OF INTERHOSPITAL TRANSFER AMONG MEDICARE BENEFICIARIES
Priya Pathak, Djhenne Dalmacy, Diamantis Tsilimigras, Madison Hyer, Adrian Diaz, Timothy M. Pawlik*
Surgery, The Ohio State Wexner Medical Center, Columbus, OH
Introduction: Not uncommonly, patients are transferred to a secondary center to help manage postoperative complications related to a procedure that occurred at a different initial hospital. The overall use and impact of interhospital transfer (IHT) to manage patients has not been well-examined. As such, we sought to define risk factors and outcomes associated with IHT following complex cancer surgery.
Methods: Medicare Inpatient Standard Analytic files were utilized to identify patients who underwent resection for esophageal, pancreatic, liver, or colorectal cancer between 2013-2017 and experienced at least one in-hospital complication. Failure-to-rescue (FTR) was defined as in-hospital mortality among patients with one or more complications. IHT was categorized as transfer to an acute care hospital (ACH) or a long-term acute care hospital (LTACH). Patient-, procedure- and hospital-level characteristics relative to IHT, as well as FTR rates following IHT were examined.
Results: Among 39,973 patients who had >1 postoperative complication following complex cancer surgery at an index hospital, 3,090 (7.7%) patients were transferred to a different secondary hospital. A subset of patients (n=210, 6.8%) had a repeat operation at the index hospital prior to IHT. Transfer to ACH was more common among patients who underwent surgery at low volume hospitals (OR 5.81, 95%CI 4.11-8.23) and individuals who experienced multiple complications (2 complications: OR 2.01, 95%CI 1.57-2.59; >3 complications: 2.36, 95%CI 1.57-2.59). In particular, compared with patients who were not transferred, IHT-ACH patients were more likely to have had a myocardial infarction (OR 4.03, 95%CI 3.04-5.34) or pulmonary failure (OR 1.52, 95%CI 1.20-1.92) at the index hospital prior to IHT. Following transfer to ACH, overall mortality was 20.2%. After adjusting for competing risk factors, patients who were transfered to an ACH had more than a 50% increased odds of FTR (OR 1.51, 95%CI 1.12-2.05) compared with non-transferred patients. Odds of FTR following IHT-ACH were more pronounced among patients who were transferred from a low volume hospital (OR: 1.45, 95%CI 1.32-1.63)(Figure). In contrast, patients who had experienced either a non-serious complication or serious complication whose care was "de-escalated" via transferred to an LTACH had a lower odds of FTR (Figure).
Conclusion: IHT was utilized in approximately 1 in 13 patients following complex gastrointestinal cancer surgery. IHT to ACH was associated with persistent high rates of FTR, especially among patients undergoing surgery at low volume hospitals. Future efforts should target strategies to optimize IHT timing and indications to improve outcomes of patients requiring higher level care.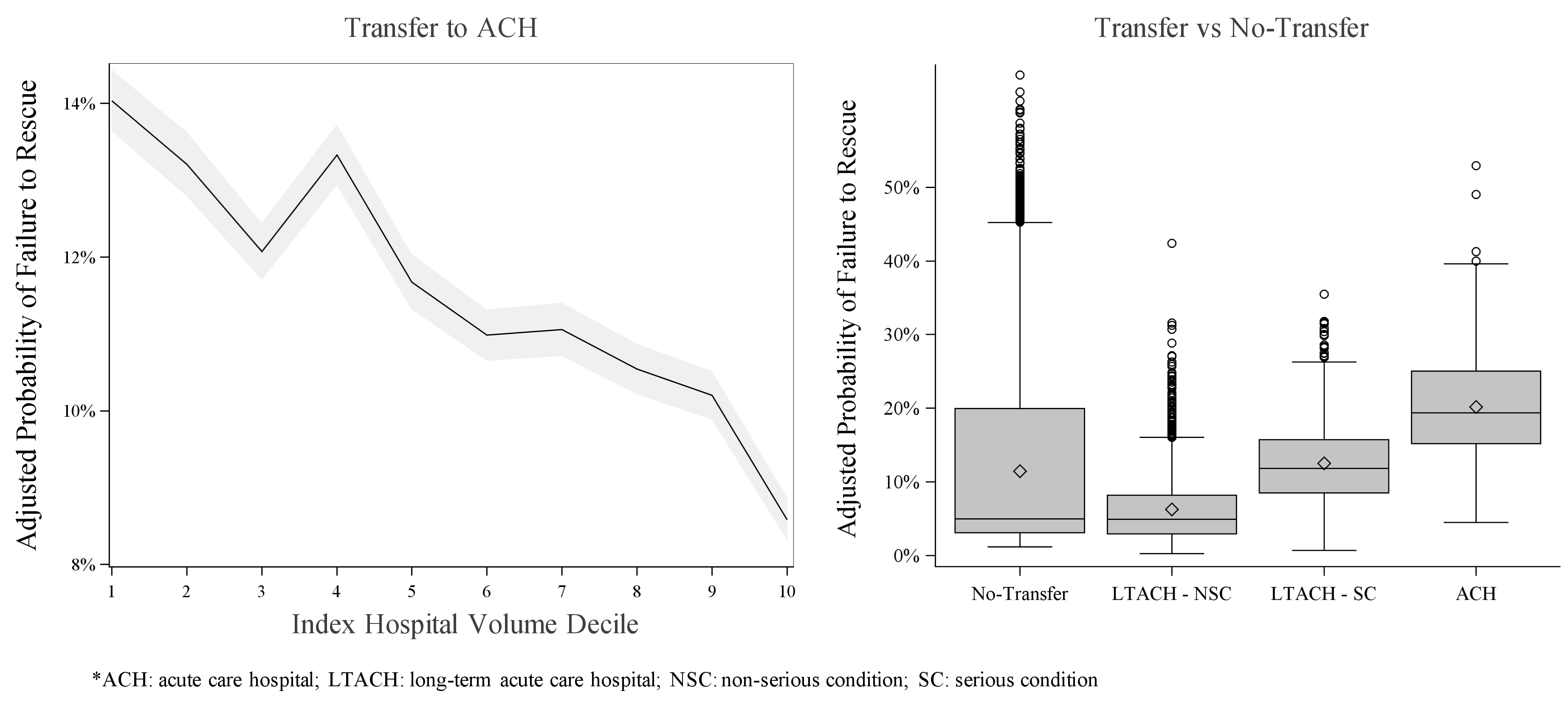
Back to 2021 Abstracts
