CLINICALLY RELEVANT PANCREATIC FISTULA FOLLOWING PANCREATODUODENECTOMY IS ASSOCIATED WITH HIGH INTRAOPERATIVE BLOOD LOSS: AN INTERNATIONAL, MULTI-INSTITUTIONAL PROPENSITY SCORE MATCHED ANALYSIS.
Fabio Casciani*1,2, Maxwell T. Trudeau1, Claudio Bassi2, Charles Vollmer1
1Hospital of the University of Pennsylvania, Philadelphia, PA; 2University of Verona, Verona, Italy
Background
The association between high intraoperative blood loss (EBL) and postoperative outcomes following pancreatoduodenectomy (PD), including clinically-relevant pancreatic fistula (CR-POPF), has been superficially explored thus far. Moreover, for obvious logistical and ethical reasons, no Level-1 evidence can be obtained from RCTs to ascertain the clinical effects of reduced EBL on CR-POPF development.
Methods
PDs performed at 18 international institutions from 2003-2020 were examined. High EBL was defined as twice the median. Postoperative results were examined, with CR-POPF being the primary outcome. Propensity score matching (PSM) with a 1:1 exact-match algorithm (caliper width=0) was employed to adjust for innate and operative variables. The study was powered to detect a 33% CR-POPF increase in the High EBL group, with α=0.05 and β=0.2.
Results
Among 7706 PDs performed, median EBL was 350mL with 1263 patients experiencing High EBL (>700mL, 16.4%). Overall, patients who experienced CR-POPF had higher median EBL [400 vs 350mL; p<0.001). After PS calculation, 966 High EBL patients were paired with 966 patients with lower EBL, with imbalance being solved for each covariate (pancreatic gland characteristics, open vs minimally invasive surgery, employed fistula mitigation strategies and surgeon's career duration; all p>0.99). In the High EBL group, the CR-POPF rate was significantly higher (19.4 vs 12.6%; p<0.001), as was grade C POPF rate (5.3 vs 2.5%; p<0.001). Additionally, all outcome metrics examined (any and severe complications, 90-day mortality, Postoperative Morbidity Index) and resource utilization (reoperation, ICU transfer, length of stay, readmission) were negatively impacted by High EBL (Table). On multivariable analysis adjusted for baseline and operative variables, High EBL was an independent predictor of CR-POPF (OR 1.78) along with prophylactic Octreotide (OR 1.95; both p<0.001), whereas increasing surgeon experience was a significant protective factor (vs '‰¤10 years, 11-20 years: OR 0.68, '‰Ą21 years: OR 0.67; p<0.05). An additional PSM analysis accounting for vascular resections was modeled, since vascular resection - a risk factor for High EBL - was associated with lower CR-POPF rates in the unmatched cohort. 1126 patients were included (563 in each arm), with balance being obtained for each predictive covariate (all p>0.99). High EBL, but not vascular resection, was confirmed as being independently associated with CR-POPF occurrence (OR 1.79; p<0.001) and resulted in poorer composite outcomes compared to low EBL cases.
Conclusion
This PSM study better establishes the relationship between greater EBL, pancreatic fistula and other outcomes following PD, where stronger evidence will not be able to be established. Minimizing blood loss is an actionable opportunity for CR-POPF reduction and surgical performance optimization.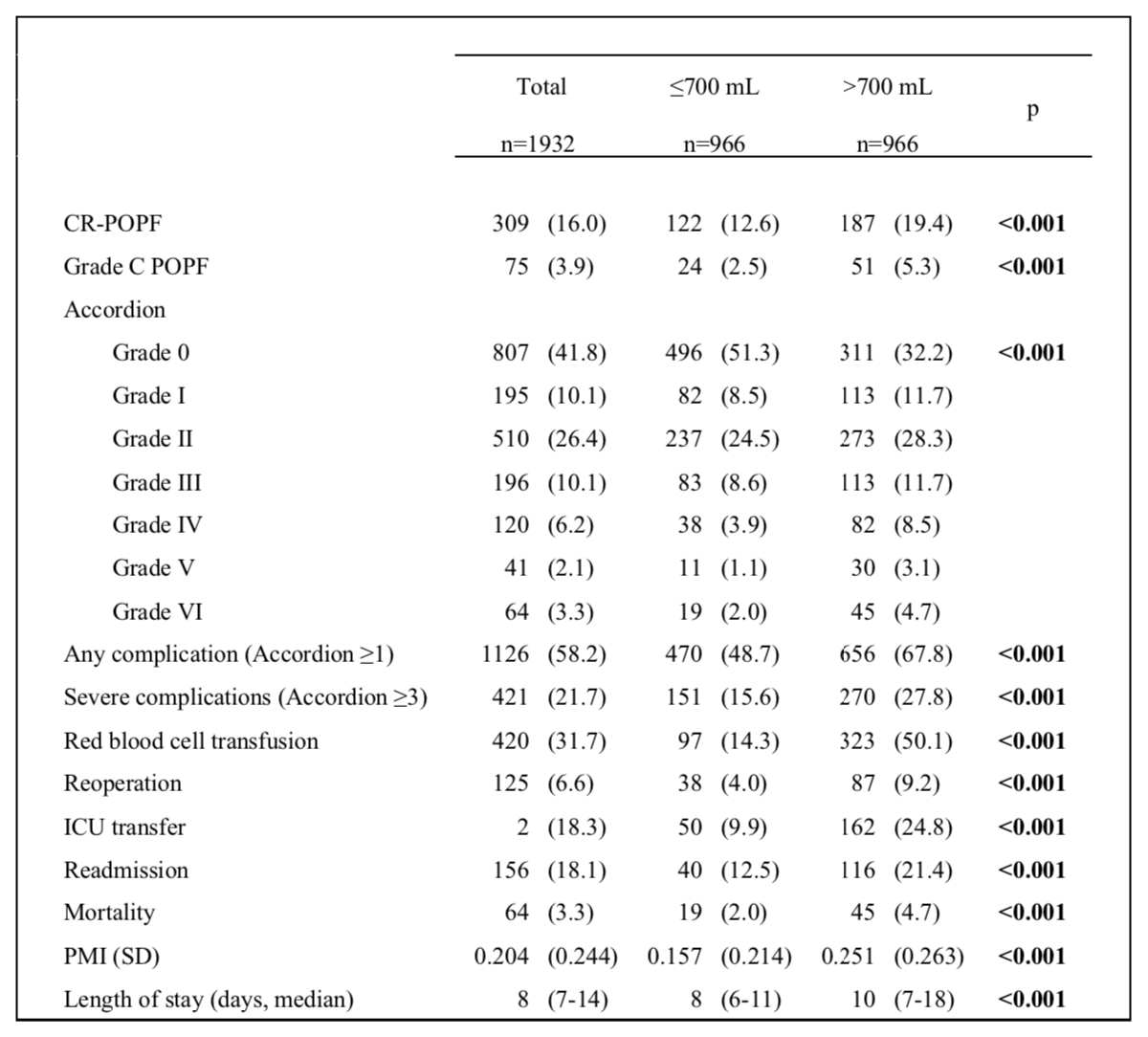
Impact of lower versus higher EBL for clinically-relevant pancreatic fistula (CR-POPF) occurrence and other postoperative outcomes in a Propensity Score Matched cohort (n=1932) derived from 7706 pancreatoduodenectomies (2003-2020) from the Pancreas Fistula Study Group collaborative.
Back to 2021 Abstracts
