OUTCOMES OF MIXED PATHOLOGIC RESPONSE IN PATIENTS WITH MULTIPLE COLORECTAL LIVER METASTASES TREATED WITH NEOADJUVANT CHEMOTHERAPY AND LIVER RESECTION
Meredith C. Mason*, Maciej Krasnodebski, Caeli Barker, Yujiro Nishioka, Anai N. Kothari, Yi-Ju Chiang, Timothy E. Newhook, Ching-Wei D. Tzeng, Yun Shin Chun, Thomas Aloia, Jean-Nicolas Vauthey, Hop Tran Cao
Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Background: Pathologic response to preoperative chemotherapy predicts survival in patients with colorectal cancer with liver metastases (CLM) who have undergone liver resection. In patients with multiple CLM, a mixed pathologic response, wherein tumors exhibit different degrees of treatment response, can be encountered. The clinical significance of this is unclear. We sought to evaluate survival outcomes of mixed pathologic response in patients with multiple CLM and to identify factors associated with mixed response.
Methods: This is a retrospective cohort study using a prospectively maintained single institution database of 444 patients with '‰¥2 CLM who underwent preoperative chemotherapy followed by hepatectomy (2010-2018). Pathologic response of each tumor was measured on permanent pathologic examination as proportion of viable tumor cells. Patients were categorized based on pathologic response in all tumors as: complete pathologic response (CR)=0-1% tumor viability; major pathologic response (MajR)=2-49% viability; minor pathologic response (MinR)=50-99% viability; mixed pathologic response (MixR)=at least one tumor with CR or MajR and at least one tumor with MinR. Standard descriptive statistics were used to describe the cohort. Multivariate logistic regression models were used to examine factors associated with MixR. Unadjusted recurrence-free survival (RFS) and overall survival (OS) were estimated using Kaplan-Meier method, and adjusted risk of death was evaluated with Cox regression.
Results: Among 444 patients, 27 (6%) had CR, 153 (34%) had MajR 158 (36%) had MinR and 106 (24%) had MixR. Factors associated with MixR included left-sided tumors [Odds Ratio (OR) 1.75 (95% Confidence Interval 1.01-3.03 vs. right-sided). Median and 5-year RFS for patients with MixR was 10.4 months and 16%, respectively, compared to patients with MajR (11.3 months and 18%), MinR (7.7 months and 13%), and CR (23.1 months and 38%), log-rank p<0.001(Figure 1A). Median and 5-year OS for patients with MixR was 77.4 months and 60%, compared to patients with MajR (80.5 months and 63%), MinR (49.9 months and 39%), and CR (37.1 months median follow up and 65%), log-rank p=0.002 (Figure 1B). After multivariate Cox regression modeling, MixR was associated with 52% reduction in risk of death [Hazard Ratio (HR) 0.48 (0.30-0.78) vs. MinR].
Conclusions: Approximately one-quarter of patients with multiple CLM have MixR following preoperative chemotherapy followed by liver resection. Although patients with MixR are a distinct group from CR, MajR, and MinR, OS and RFS for patients with MixR approach those of MajR rather than MinR, suggesting the greatest response achieved in any metastases best predicts survival rather than the poorest response. MixR may serve as an important prognostic indicator and may be used to inform postoperative therapy in the future.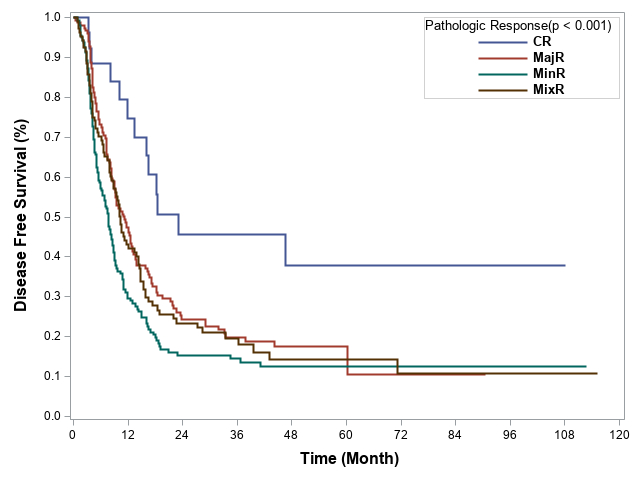
Recurrence-Free Survival, by pathologic response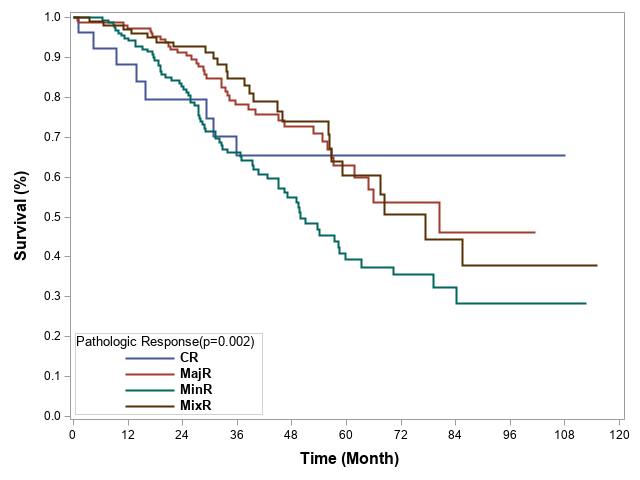
Overall Survival, by pathologic response
Back to 2021 Abstracts
