INTRA-OPERATIVE BILE CULTURE IN PANCREATICODUODENECTOMY: TEACHING OLD DOGMA NEW TRICKS
Thomas L. Sutton*, Jack P. O'Grady, Robert G. Martindale, Skye C. Mayo, Erin Gilbert, Brett C. Sheppard
Surgery, Oregon Health and Science University, Portland, OR
Introduction:
Biliary stents increase the risk of surgical site infections (SSI) following pancreaticoduodenectomy due to bactibilia and contaminated intra-operative bile spillage. Intra-operative bile culture (IOBC) is sometimes performed to guide postoperative antibiotic therapy for SSIs, however the utility of this practice is poorly studied. We sought to characterize the utility of IOBC and the interplay between stenting, bactibilia, and SSI following pancreaticoduodenectomy in a high-volume pancreatic care center.
Methods:
Patients undergoing pancreaticoduodenectomy from January 2008 to April 2020 were identified through our institutional National Surgical Quality Improvement Project (NSQIP) and cancer databases. Bile culture from the transected common bile duct were taken following stent removal, and IOBC results were collected; NSQIP-defined SSIs were analyzed with binomial logistic regression in a univariate a multivariate setting.
Results:
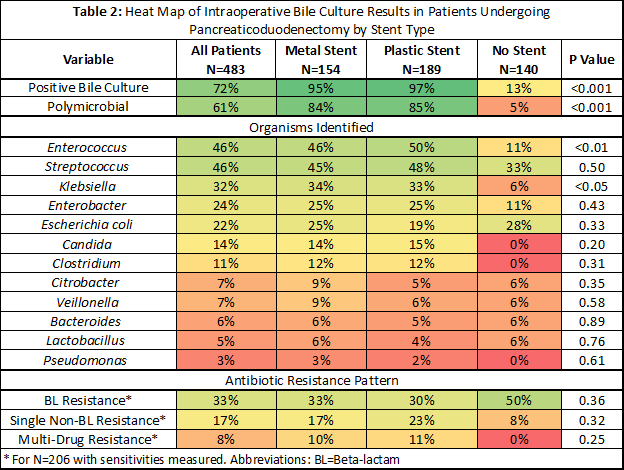
Of 655 patients undergoing pancreaticoduodenectomy, 483 (74%) had IOBC and were included in the study; median patient age was 67 years. 189 (39%) patients had plastic stents, 154 (32%) had metal stents, and 140 (29%) were not stented; stent groups differed in several clinicopathologic characteristics (Table 1). 329 (96%) patients with stents had bactibilia, compared to 18 (13%) without stents (P<0.001). The biliary microbiome and antibiotic resistance patterns in patients with metal and plastic stents were nearly identical, but collectively differed from patients without a biliary stent (Table 2).
Overall, 159 (33%) experienced an SSI, most commonly incisional (n=92, 22%). On multivariable regression controlling for relevant demographic, comorbidity, and operative characteristics, monomicrobial and polymicrobial bactibilia were independently associated with incisional SSI (OR 3.46 and 4.01, both P<0.01) but not organ space SSI (P>0.1). Stent type was not independently associated with odds of incisional or organ space SSI beyond associated bactibilia (P>0.5). Of 73 patients with speciated cultures from a SSI, 39 (53%) were polymicrobial; at least one organism identified from IOBC was present in 42 (58%), while at least one organism not identified on IOBC was present in 49 (67%).
Conclusion:
Bactibilia is independently associated with incisional but not organ space SSI following pancreaticoduodenectomy and is strongly associated with stent presence. The decision for metal versus plastic stent placement should not be influenced by infectious concerns, as stent composition is not an independent risk factor for SSI and is not associated with unique biliary microbiomes or antibiotic resistance patterns. IOBC has a poor ability to predict causative organisms in SSI following pancreaticoduodenectomy, missing a causative organism in two-thirds of cases. IOBC is therefore not recommended for routine use.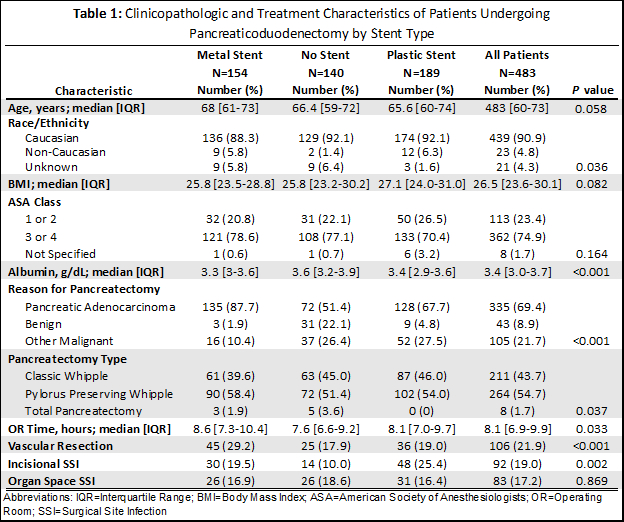
Back to 2021 Abstracts
