OBESITY WORSENS LOCAL AND SYSTEMIC COMPLICATIONS OF NECROTIZING PANCREATITIS AND PROLONGS DISEASE COURSE
Sean P. McGuire*1, Sydney L. Keller1, Thomas K. Maatman1, Kyle A. Lewellen1, Stephen N. Quigley2, Eugene P. Ceppa1, Michael G. House1, Attila Nakeeb1, Trang K. Nguyen1, Christian Schmidt1, Nicholas J. Zyromski1
1Indiana University School of Medicine, Indianapolis, IN; 2Eastern Health, St. John's, , Canada
Introduction:
Obesity is epidemic in the United States. Existing evidence suggests that obesity increases the incidence of acute pancreatitis (AP) and worsens AP severity. Limited data exist examining obesity in necrotizing pancreatitis (NP).
Methods:
Retrospective review of prospectively maintained database of 571 adult necrotizing pancreatitis patients in a single institution between 2007 and 2018. Weights closest to disease onset and disease resolution were recorded. Patients were grouped according to body mass index (BMI) at disease onset. Patient characteristics, necrotizing pancreatitis course, and outcomes were compared between non-obese (BMI <30) and obese (BMI >30) patients.
Results:
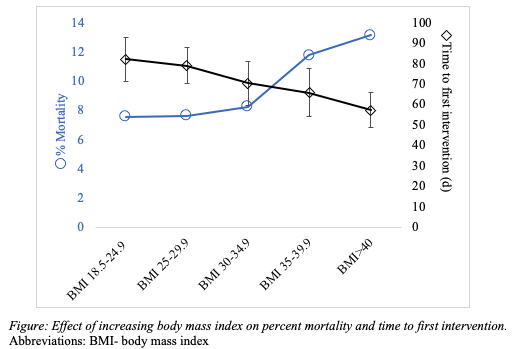
Among 536 patients with BMI data available, 232 (43%) were non-obese (BMI<30) and 304 (57%) were obese (BMI >30). Age and sex were similar between groups. NP etiology in the obese group was more commonly biliary (55% vs 46%, p = 0.04) or secondary to hypertriglyceridemia (10% vs 2%, p < 0.001) and less commonly alcohol (17% vs 26%, p = 0.01). Obese patients had a higher incidence of baseline coronary artery disease (15% vs 7%, p = 0.005), atrial fibrillation (6% vs 2%, p = 0.02), hypertension (66% vs 53%, p = 0.004), hyperlipidemia (41% vs 28%, p = 0.003), diabetes mellitus (31% vs 19%, p = 0.001), and obstructive sleep apnea (7% vs 0.9%, p <0.001). The CT severity index was similar between groups (Table), though obese patients had a higher rate of >50% pancreatic gland necrosis (27% vs. 19%, p = 0.02). The rates of infected necrosis and organ failure were higher among obese patients (Table). NP disease duration was longer in obese patients (Table). Percutaneous drainage was more common in obese patients, but no other differences in NP interventions were observed (Table). The overall mortality rate of non-obese and obese patients did not differ (Table). However, mortality increased with increasing BMI and time to first necrosis intervention decreased with increasing BMI (Figure). These results did not achieve statistical significance.
Conclusion:
Necrotizing pancreatitis in obese patients is characterized by a prolonged disease course. Obese patients with necrotizing pancreatitis are at higher risk for organ failure, infected necrosis, and the need for early necrosis-related intervention.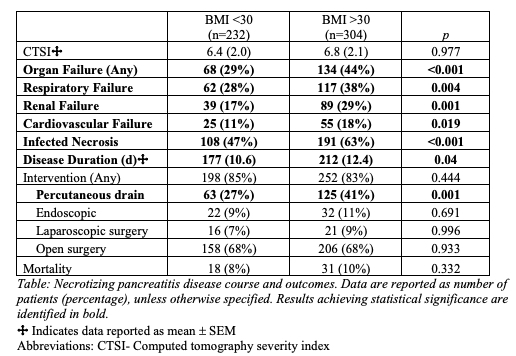
Back to 2021 Abstracts
