NATIONWIDE EXPERIENCE OF TOTAL PANCREATECTOMY WITH ISLET CELL AUTOTRANSPLANT FOR CHRONIC PANCREATITIS: BENCHMARK METRICS AND TRENDS IN OUTCOMES
Thomas K. Maatman*1, Sean P. McGuire1, Kathleen A. McGreevy2, Evan L. Fogel1, Michael G. House1, Nicholas J. Zyromski1
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University Health Inc, Indianapolis, IN
Introduction:
Total pancreatectomy with islet cell autotransplant (TP-IAT) is increasingly performed for patients with small duct or genetic chronic pancreatitis (CP). This complex procedure is performed at a small number of highly experienced pancreatic centers; postoperative outcomes after TP-IAT have not been systematically evaluated at a national level. The aim of this study was to evaluate frequency and risk factors for major morbidity and mortality after TP-IAT. We hypothesized that postoperative outcomes have improved over time with increasing utilization of TP-IAT for chronic pancreatitis.
Methods:
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) Participant Use Files (PUF) were queried to identify patients undergoing TP-IAT for CP between 2006 and 2018. Major morbidity was defined as Clavien-Dindo grade III or higher level complications. Incidence and risk factors for major morbidity and mortality were evaluated with the chi-squared test, Student's t-test, and multivariable binary logistic regression. P values < 0.05 were accepted as statistically significant.
Results:
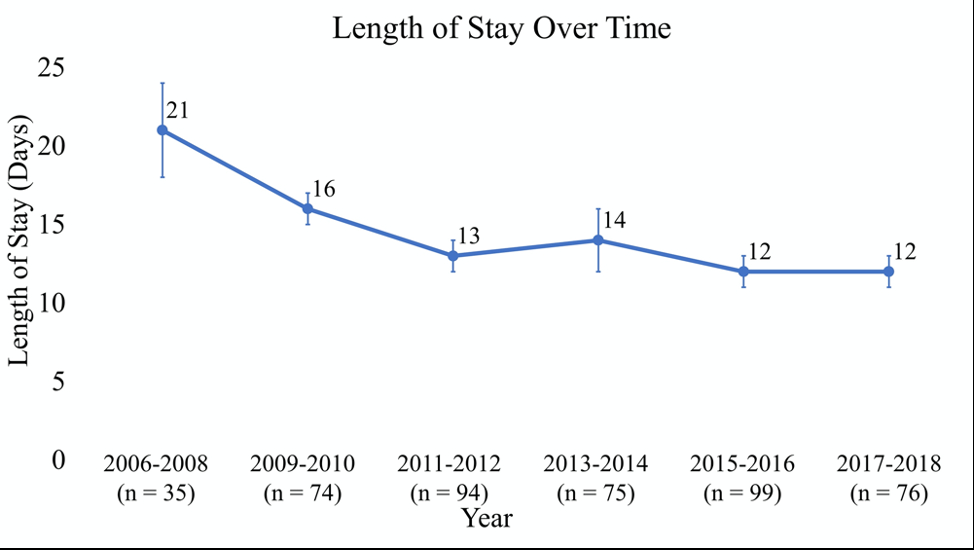
A total of 453 patients underwent TP-IAT. The mean age was 42'±12 years and 68% of patients were female. Major postoperative morbidity developed in 88 (19%) patients and most commonly included unplanned repeat operation (n = 56, 12%), organ space surgical site infection (n = 39, 9%), and failure to wean from mechanical ventilation (n = 19, 4%). Multivariable analysis identified increasing age (OR, 1.024; 95% CI, 1.003-1.046; p = 0.027) and operative time (OR, 1.12; 95% CI, 1.0003-1.236; p = 0.049) as independent risk factors for postoperative major morbidity. No differences in postoperative outcomes were observed between patients with and without pancreatic endocrine insufficiency. After TPIAT, significant improvements in major morbidity (p = 0.030) and length of stay (p < 0.0001) were observed over the duration of the study (Figures 1 and 2). Thirty-day mortality was 0.2% (one patient).
Conclusion:
In this large, national cohort of patients, total pancreatectomy with islet cell autotransplantation was performed safely and with acceptable rates of major morbidity. Major morbidity and postoperative length of stay have improved significantly over time.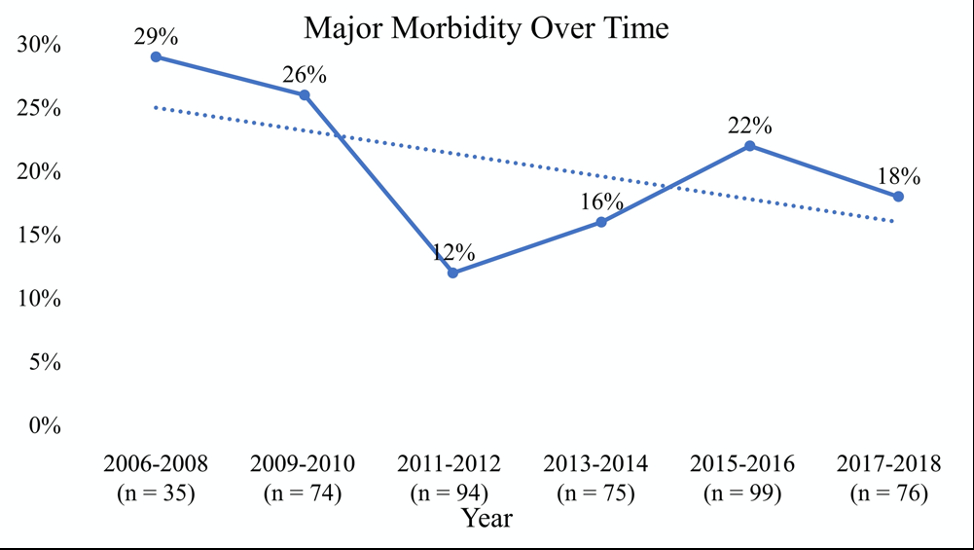
Back to 2021 Abstracts
