RURAL HOSPITALS ARE NOT ASSOCIATED WITH WORSE POSTOPERATIVE OUTCOMES FOR COLON CANCER
Adrian Diaz*, Madison Hyer, Diamantis Tsilimigras, Shan Lansing, Matthew Kalady, Syed Husain, Alan Harzman, Alessandra Gasior, Lisa Cunningham, Emily Huang, Mark Arnold, Timothy M. Pawlik
Surgery, The Ohio State Wexner Medical Center, Columbus, OH
Introduction:Regionalization of high-risk operations has been proposed to improve postoperative surgical outcomes. Patients living in rural areas may be disproportionally affected by regionalization of care to urban centers, leading to disparities in access. We sought to characterize postoperative outcomes among patients living in rural areas who underwent colon cancer surgery at rural versus non-rural hospitals.
Methods:Medicare beneficiaries who underwent colon resection for cancer between 2016-2017 were identified using the 100% Medicare Inpatient Standard Analytic Files. Patients and hospitals were designated as rural based on county and rural-urban continuum codes. Risk-adjusted postoperative outcomes and hospitalization spending were compared among patients undergoing resection at rural versus non-rural hospitals.
Results:Among 969 Medicare beneficiaries who lived in rural areas and underwent colon resection for a malignant indication, mean age was 76.3 years (SD:7.3) and the overwhelming majority were White (n= 907, 93.6%). Overall, 866 (89.4%) patients underwent colectomy at a non-rural hospital, while 103 (10.6%) patients had surgery at a rural hospital. Age and sex were similar among patients who had an operation at rural versus non-rural hospitals (p>0.05); however, more patients with >3 comorbidities were treated at non-rural hospitals (rural: n=69, 67.0% vs. non-rural: n=665, 76.8%; p=0.02). Tumor location (rural: right colon, n=65, 63.1% vs. non-rural: right colon, n=500, 57.7%), as well as surgical approach (rural: MIS, n=26, 25.2% / open, n=77, 74.8% vs. non-rural: MIS, n=287, 33.1% / open, n=579, 66.9%) was similar among patients who underwent colon resection at rural and non-rural hospitals (all p>0.05)(Table). Risk-adjusted probability of postoperative complications was similar among non-rural and rural hospitals (OR:1.15, 95%CI 0.52-2.54). Similarly, there were no differences in risk-adjusted length-of-stay (OR:0.02, 95%CI 0.09-0.12), failure-to-rescue (OR: 1.41 95%CI 0.32-6.28), 30-day readmission (OR:1.07 95%CI 0.47-2.44), or 30-day mortality (OR:2.47 95%CI 0.57-10.75). Costs at rural hospitals ($15,999) were, however, lower than at non-rural centers ($18,266)(OR:-0.13, 95%CI -0.25--0.01; p=0.02).
Conclusion: Among rural Medicare beneficiaries who underwent a colon resection for cancer, there were no differences in postoperative outcomes among non-rural versus rural hospitals. The findings highlight the importance of selective regionalization and serve to emphasize that not all cancer operations may need to be targeted for such initiatives. Colon resection performed at rural hospitals was both safe and associated with lower costs, perhaps representing a better value proposition for select patients.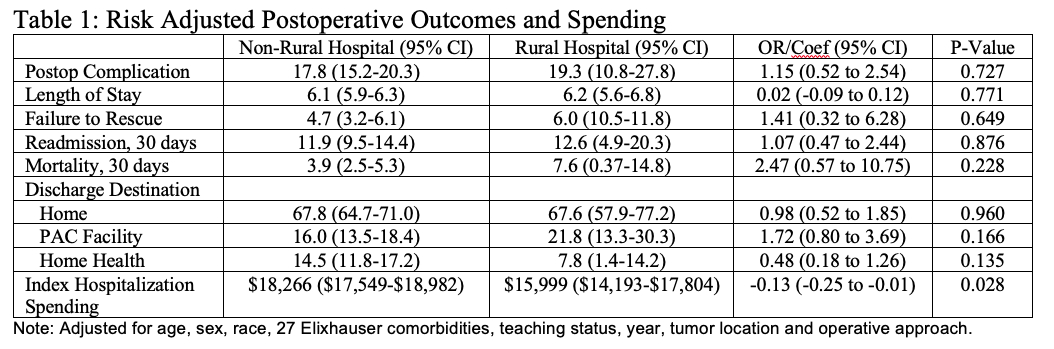
Back to 2021 Abstracts
