VALIDATION OF THE PITTSBURGH SEVERITY SCORE IN DETERMINING THE CLINICAL OUTCOME AFTER ESOPHAGEAL PERFORATION: A SINGLE CENTER EXPERIENCE
Lucia Moletta*, Giovanni Capovilla, Elisa Sefora Pierobon, Giovanni Valotto, Laura Gavagna, Gianpietro Zanchettin, Renato Salvador, Mario Costantini, Stefano Merigliano, Michele Valmasoni
Universita degli Studi di Padova, Padova, Veneto, Italy
Background
Esophageal perforation (EP) is a challenging surgical emergency, characterized by high morbidity and mortality. Recently, beyond the traditional surgical approaches, several studies have reported successful management through nonoperative treatment in selected patients. However, there is a lack of consensus to guide patients' management. In 2009, the Pittsburgh group proposed a perforation severity score (PSS) based on clinical variables to stratify patients predicting their outcome. The aim of this study was to verify PSS usefulness in stratifying EP severity and in guiding clinical decision making.
Methods
We enrolled consecutive patients referred to our Unit for EP between May 2005 and September 2020. Data on clinical presentation, management and outcomes were recorded prospectively on a dedicated database. Patients were stratified according to their PSS at presentation into 3 groups (< 2; 3-5 and > 5): the postoperative outcomes were compared between the 3 groups by univariated analysis. The predictive value of the PSS was evaluated by means of simple linear and logistic regression for the following outcome: overall and postoperative complications, in-hospital mortality, ICU and hospital stay, time to refeeding, need for surgical treatment and reoperation.
Results
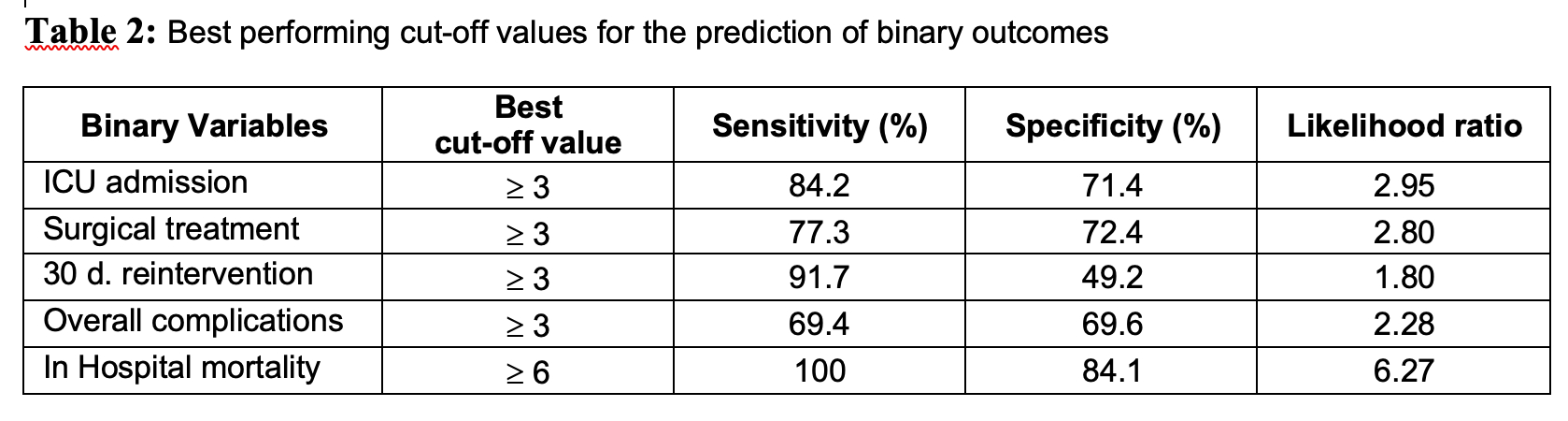
Seventy-three patients were referred to our Unit for EP (M/F: 46/27, median age 67 yr). Most perforations occurred at the gastroesophageal junction and were mainly iatrogenic (30/73, 41%) and spontaneous (27/73, 37%). The median PSS was 4 (IQR 2-6), the distribution of patients in the 3 groups (< 2; 3-5 and > 5) was 31, 27 and 15 patients, respectively. Surgical treatment was required in 61.4% of cases while the remaining were treated conservatively. Median length of stay was 19 days (range 5-221). Thirty-eight patients required ICU admission, with a median ICU stay of 5 days (range 1-210). Overall post-perforation morbidity rate was 67.1%. Overall in-hospital mortality was 6.1%. Table 1 summarizes the association between PSS and outcomes in univariated analysis. After logistic or linear regression analysis, PSS was significantly predictive of post-perforation complications (p<0.01); in-hospital mortality (p<0.01); ICU admission (p<0.01); need for surgical treatment (p<0.01) and for reintervention (p=0.02). Furthermore, the performance of PSS of the above mentioned outcomes was assessed by means of Receiver-operator curve (ROC) analyses; the best performing cut-off values for outcome prediction are reported in Table 2.
Conclusion
According to our results, the PSS is a reliable scoring system, useful in assessing the severity and potential consequences of EP and in stratifying patients in risk groups with different morbidity and mortality outcomes. Prospective studies are needed to establish the role of the PSS in the treatment of esophageal perforation.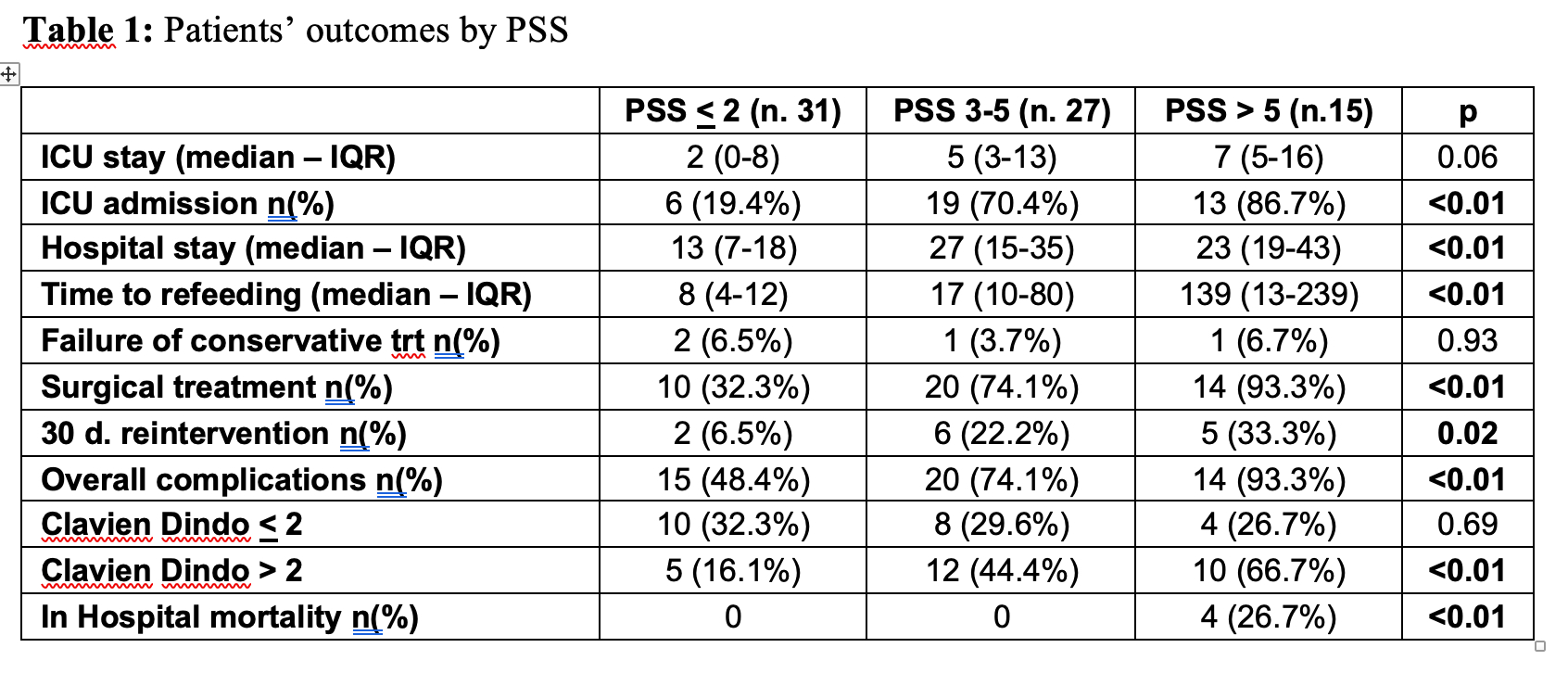
Back to 2021 Abstracts
