THE CONTRIBUTION OF SURGEON AND HOSPITAL VARIATION IN TRANSFUSION PRACTICE TO OUTCOMES FOR PATIENTS UNDERGOING GASTROINTESTINAL CANCER SURGERY: A POPULATION-BASED ANALYSIS
Jesse Zuckerman*1, Natalie Coburn1,2, Jeannie Callum2, Alyson L. Mahar3, Robin Mcleod1, Emily Pearsall6, Yulia Lin2, Alexis F. Turgeon4, Guillaume Martel5, Julie Hallet1,2
1Surgery, University of Toronto, Toronto, ON, Canada; 2Sunnybrook Health Sciences Centre, Toronto, ON, Canada; 3University of Manitoba, Winnipeg, MB, Canada; 4Universite Laval, Quebec, QC, Canada; 5University of Ottawa, Ottawa, ON, Canada; 6University of Toronto, Toronto, ON, Canada
Introduction: Patients undergoing gastrointestinal (GI) cancer surgery often receive red blood cell transfusions (RBCT). RBCT are a scarce and costly resource that have been associated with morbidity, mortality, and cancer recurrence. RBCT have been targeted as an overused treatment, warranting minimization of their use. Despite level-1 evidence and practice guidelines informing transfusion practice, significant practice variation persists. We examined the association between surgeon and hospital variation in transfusion practice with post-operative major morbidity and mortality in patients undergoing GI cancer surgery.
Methods: We performed a population-based cohort study of patients undergoing elective GI cancer resection over 2007-2019. Hierarchical logistic regression models estimated case-mix-adjusted RBCT and 90-day morbidity or mortality rates for each surgeon and hospital. Correlations between physician- and hospital-level RBCT and morbidity/mortality rates were assessed. Odds ratios (OR) and R2-measures assessed the contribution of surgeon- and hospital-level RBCT variation to morbidity and mortality.
Results: 59,964 patients (median age 69 years; 43.2% female; 75.8% colorectal resections), 81 hospitals, and 616 surgeons were included. 18.0% of patients received RBCT. Adjusted RBCT rates ranged from 7.4-36.4% for surgeons and 8.4-30.0% for hospitals. Surgeon-level RBCT rates were weakly correlated with 90-day major morbidity (Ï?=0.17, p<0.001), whereas hospital-level rates were not (Ï?=0.15, p=0.19) (Figure 1). 90-day mortality was correlated with both surgeon- (Ï?=0.18, p<0.001) and hospital-level RBCT rates (Ï?=0.23, p=0.035) (Figure 2). While surgeon-level RBCT rates contributed to 1.6% of the explained variation in morbidity and 0.7% to the variation in mortality, rising surgeon-level RBCT rates were independently associated with higher odds of morbidity and mortality. For every 5% increase in surgeon-level RBCT rate, the odds of morbidity and mortality increased by approximately 10% (90-day morbidity: OR 1.10, 95% CI 1.07-1.14); 90-day mortality: OR 1.09, 95% CI 1.05-1.14) adjusted for case-mix. Hospital-level RBCT rates were not associated with morbidity or mortality and contributed minimally to their explained variation.
Conclusions: We observed a wide variation in surgeon and hospital transfusion practices that were associated with patient outcomes. After adjusting for case mix, patients of surgeons who transfused fewer patients overall had better outcomes. Individual transfusion practices are a potentially modifiable process of care that should be targeted by quality improvement programs, including monitoring and reporting, with a goal of standardizing perioperative transfusion practices to improve patient outcomes.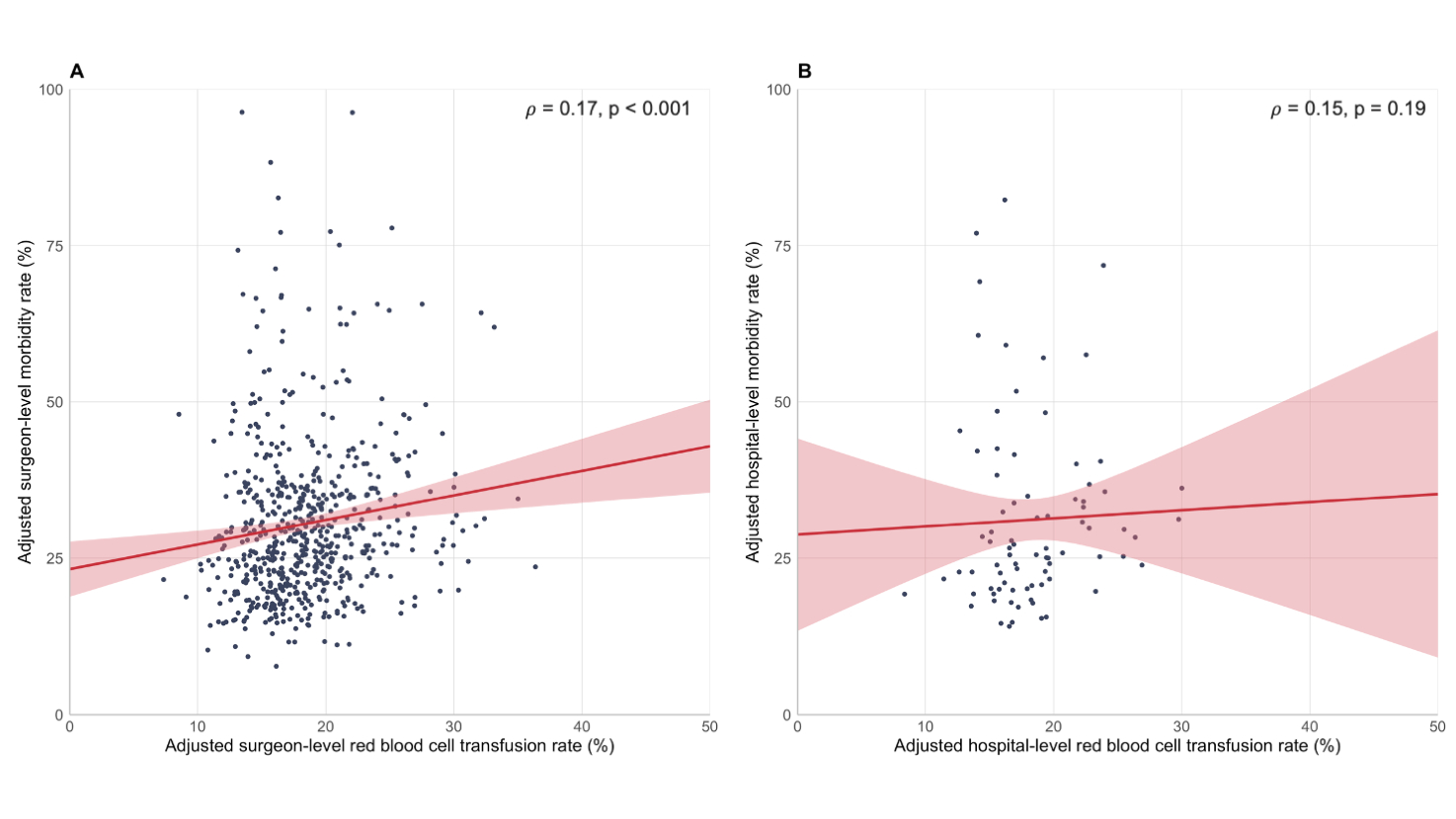
Figure 1: Association between physician- and hospital-level red blood cell transfusion rates and 90-day morbidity (A: surgeon, B: hospital)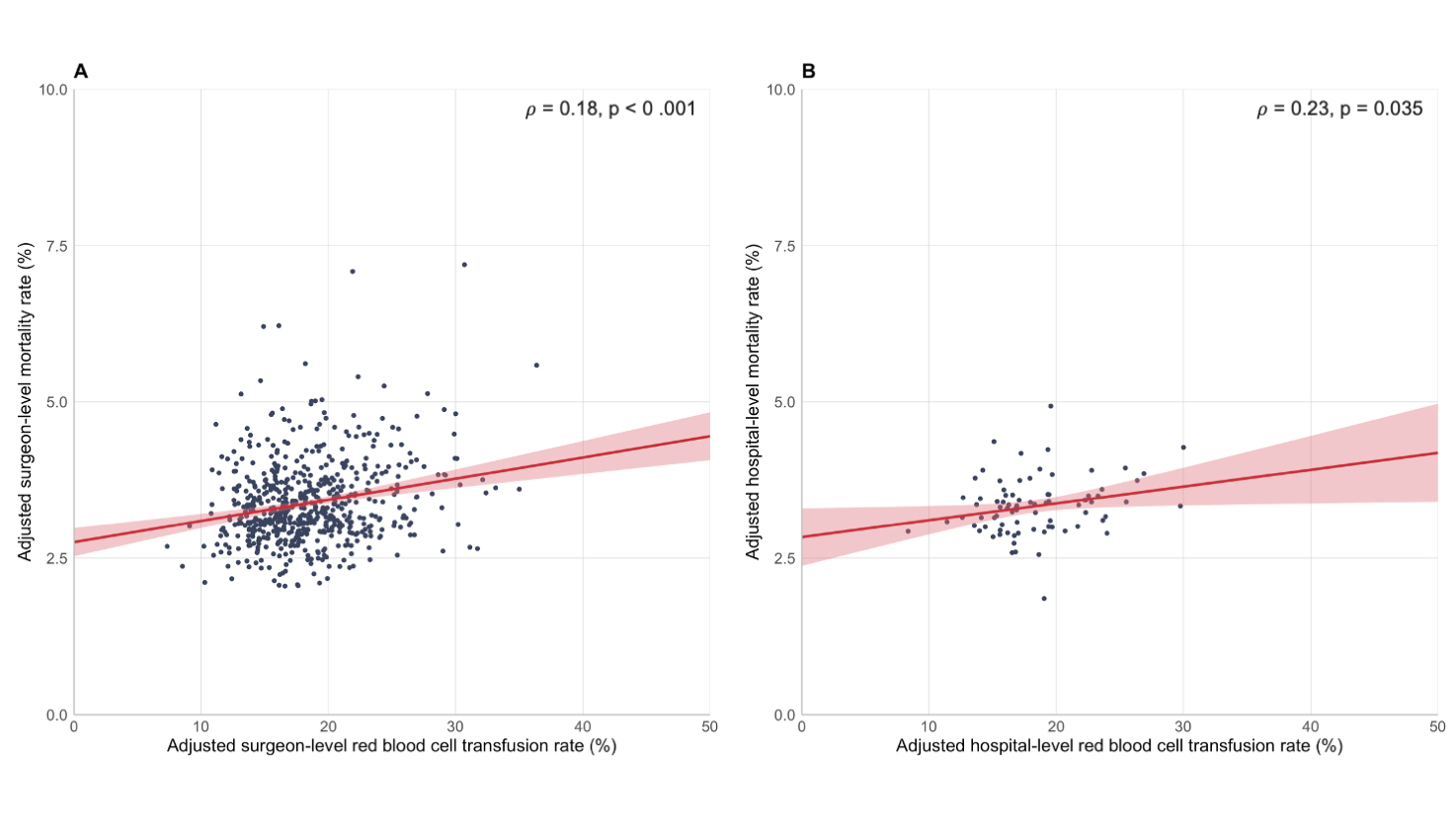
Figure 2: Association between physician- and hospital-level red blood cell transfusion rates and 90-day mortality (A: surgeon, B: hospital)
Back to 2021 Abstracts
