IBD-ASSOCIATED COLORECTAL CANCER HAS SIMILAR CHARACTERISTICS AND OUTCOMES COMPARED TO SPORADIC CRC.
Yasmeen Z. Qwaider*, Naomi M. Sell, Chloe Boudreau, Rocco Ricciardi, Liliana G. Bordeianou, Christy E. Cauley, Richard A. Hodin, David L. Berger, Hiroko Kunitake, Robert N. Goldstone
Massachusetts General Hospital, Boston, MA
Introduction
Inflammatory bowel disease (IBD) accounts for around 1-2% of all colorectal cancer (CRC). Contrary to prior reports, two recent studies demonstrated decreased survival in patients with IBD-associated CRC compared to sporadic CRC. This study assesses the variations and similarities in clinicopathological characteristics, treatment courses and outcomes between IBD-associated CRC and sporadic CRC, in an attempt to resolve these differences.
Methods
Data was retrospectively extracted and analyzed from our institutional database containing all patients with surgically resected CRC between 2004 and 2015. Patients were divided into 2 groups, those with IBD-associated CRC and those with sporadic CRC. We then compared the clinicopathological variables, course of treatment and outcomes between both groups.
Results
Of the 1,515 patients included in this analysis, 50 carried a diagnosis of IBD (3%). Twenty-six patients had Crohn's disease (64%) and 24 had UC (48%). The average age at CRC diagnosis was 62.2 for IBD-associated CRC and 65.2 for sporadic CRC (p=0.2). Patients with IBD-associated CRC were more likely to receive total proctocolectomies than patients with sporadic CRC (p<0.001), although segmental resections were still the most common procedure in both groups. Patients with sporadic CRC were more likely to present with metastatic disease (p=0.05). In addition, patients with IBD-associated CRC were less likely to have rectal tumors and more likely to have synchronous tumors (p<0.001). There was no significant difference in administration of neoadjuvant and adjuvant chemotherapy (p=0.3 and p=0.2, respectively). Sub-analysis for patients with additional histopathological data showed that there was no significant difference between patients with IBD-associated CRC and sporadic CRC with respect to extramural vascular invasion, post-operative histopathological diagnosis, rate of r0 resections, tumor grade or perineural invasion (p>0.05). There was no significant difference in survival between patients with IBD-related CRC and sporadic CRC across all stages (p=0.5). On multivariable Cox regression analysis, IBD was not an independent prognostic factor for overall survival (aHR=1.2, CI=0.6-2.3, p=0.6)
Conclusions
Patients with IBD-related CRC have similar clinical characteristics and oncologic outcomes compared to patients with sporadic CRC while controlling for age.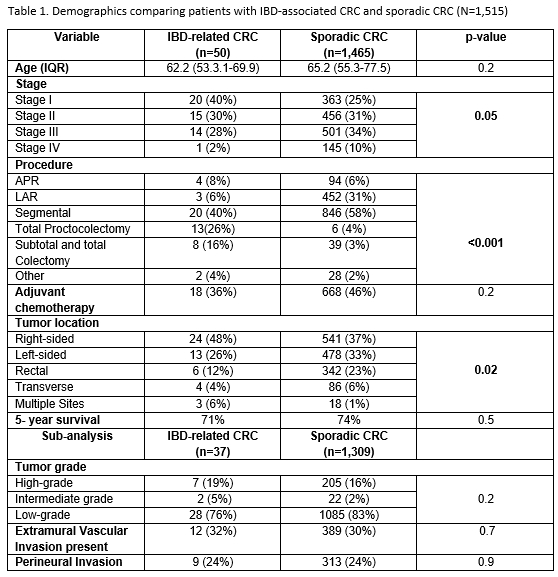
Back to 2021 Abstracts
