FACTORS ASSOCIATED WITH READMISSIONS AFTER COLORECTAL RESECTION WITH A STOMA. IS THERE A DIFFERENCE BETWEEN COLOSTOMY AND ILEOSTOMY?
Alexander A. Hart*1, Paolo Goffredo2, Asgeir Masson3, Jacklyn M. Engelbart3, Edward Cho3, Catherine Tran3, Sajida Ahad3, Imran Hassan3
1Roy J. and Lucille A. Carver College of Medicine, University of Iowa, Iowa City, IA; 2University of Minnesota Department of Surgery, Minneapolis, MN; 3Department of Surgery, University of Iowa Hospitals and Clinics, Iowa City, OR
Background: The need for an ostomy following colorectal resections is determined by patient, disease, and intraoperative factors. Patients undergoing a diverting or end colostomy or ileostomy have been shown to have increased perioperative morbidity, including hospital readmissions. The current study aimed to 1) Determine the overall incidence rates of post-operative readmissions following colorectal resection with stoma, focusing on differences between ileostomy vs colostomy, and 2) Identify risk factors for readmission.
Methods: Adult patients undergoing a colorectal resection with an ostomy were identified from the ACS-NSQIP database (2016-2018). Primary CPT codes for segmental colectomy, total colectomy, proctectomy, or proctocolectomy, with a defined colostomy or ileostomy in the code description met inclusion criteria. Multivariate analyses were conducted utilizing 30-day readmission and post-operative grade 3 complications as outcome measures.
Results: A total of 34,525 patients were identified, of which 74% and 26% underwent a colostomy and ileostomy, respectively. The median age was 63 years (IQR:52-73), median body mass index was 27 (IQR:24-32) with 49% being female. Median length of stay was 7 days (IQR: 5-11). In the unadjusted comparison colorectal resection and a colostomy had a lower readmission rate (12%) as compared to an ileostomy (16%). Factors independently associated with 30-day readmission were younger age, female sex, diabetes, ASA '‰¥3, primary procedure of proctectomy or proctocolectomy, discharge to home and having a grade 3 complication before or after discharge (Table 1). However ostomy type, surgical indication, and laparoscopic approach did not independently impact readmission. The overall rate of grade 3 complications in the cohort was 32%, and was associated with younger age, male gender, weight loss, obesity, smoking, benign indication, emergency status, longer operative time, having a concomitant secondary procedure, and a discharge destination other than home. The risk of complications was decreased by a laparoscopic approach but was not associated with the type of ostomy.
Conclusions: In patients undergoing colorectal resection and a stoma the type of ostomy performed was not a significantly associated with 30-day readmissions. Almost one-third of patients in this cohort had a major complication, which was the most significant factor associated with readmission. Patients with an ostomy following colorectal resections are at risk for perioperative complications and readmissions and represent a high risk group. Strategies to decrease perioperative complications, and to manage them when they occur, represent areas of process improvement to mitigate readmissions.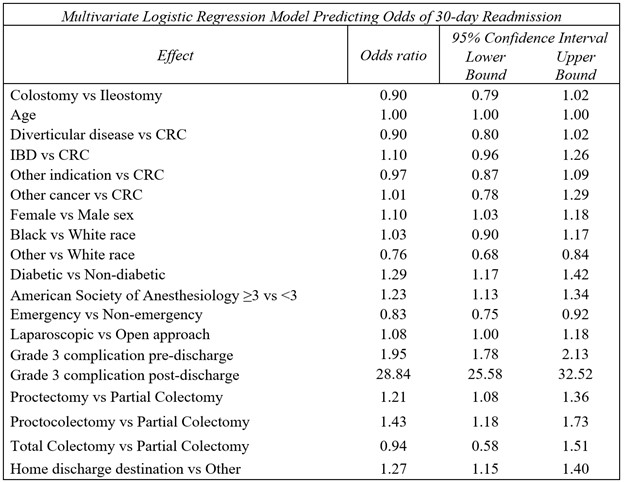
Multivariate logistic regression was conducted with 30-day readmissions as the outcome. Variables were selected through forward selection with an alpha value of less than 0.2 for entry.
Back to 2021 Abstracts
