LOW-DOSE ASPIRIN FOR EXTENDED VENOUS THROMBOEMBOLISM PROPHYLAXIS AFTER INFLAMMATORY BOWEL DISEASE SURGERY: IS IT A COST-EFFECTIVE ALTERNATIVE TO ENOXAPARIN?
Ira Leeds*, Bradford Sklow, Emre Gorgun, David Liska, Amy L. Lightner, Tracy L. Hull, Scott Steele, Stefan D. Holubar
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
Purpose and Background
Cost-effectiveness models have challenged current guidelines recommending venous thromboembolism extended prophylaxis (VTE ePPx) after inflammatory bowel disease (IBD) surgery due to the low absolute rates of VTE and high costs of post-discharge medication regimens. The purpose of this study was to evaluate if adopting an aspirin-based ePPx strategy may address the cost-effectiveness limitations of enoxaparin.
Methods
We constructed a decision analysis model to compare costs and outcomes of a reference case 37-year-old patient undergoing IBD-associated colorectal surgery considered for post-discharge VTE ePPx. In the first-round of modeling, we tested whether low-dose aspirin was superior to an enoxaparin regimen. If aspirin was the superior cost-effective option, we planned a second-round decision model comparing aspirin to no ePPx. The post-discharge VTE risk (1.1%), aspirin and enoxaparin ePPx efficacy for prevention of VTE (RR = 0.70, 0.55, respectively), bleeding risks (0.8%, 1.3%, respectively), and post-VTE sequelae were obtained from source literature. Total health care costs and benefits (quality-adjusted life years, QALYs) were used to reflect a healthcare sector perspective (3% discounting) model. Given aspirin's over-the-counter accessibility, we also assessed cost-effectiveness from a patient-perspective model. For all analyses, we performed a 10,000-simulation Monte Carlo probabilistic sensitivity analysis to account for uncertainty in model estimates.
Results
The results of each model tested are reported in Table 1. Enoxaparin compared to aspirin demonstrated an unfavorable incremental cost-effectiveness ratio (ICER) of $908,268 per QALY (conventional willingness to pay threshold: $150,000 per QALY). Sensitivity analysis supported this finding in over 75% of simulated cases; scenarios favoring enoxaparin included those with >4% post-discharge VTE rates.
When comparing aspirin to no ePpx, the aspirin strategy demonstrated a favorable ICER of $106,601 per QALY (43% agreement with sensitivity simulations, Figure 1). The findings were vulnerable to scenarios where post-discharge VTE rate <1%, aspirin-associated bleeding rate >1%, hospital costs of bleeding > 3X the mean, and decreased efficacy of aspirin (RR > 0.75). For the patient's out-of-pocket costs perspective, the QALYs remained constant but cost per QALY decreased by 66% compared to all-payer costs. The average out-of-pocket cost of choosing an aspirin ePPx strategy increased by $54 per patient versus $708 per patient with enoxaparin.
Discussion
Low-dose aspirin VTE extended prophylaxis following IBD surgery has a favorable cost and safety profile compared to enoxaparin or no prophylaxis strategies and thus may be an attractive alternative strategy. Further research is needed to determine its efficacy in this patient population.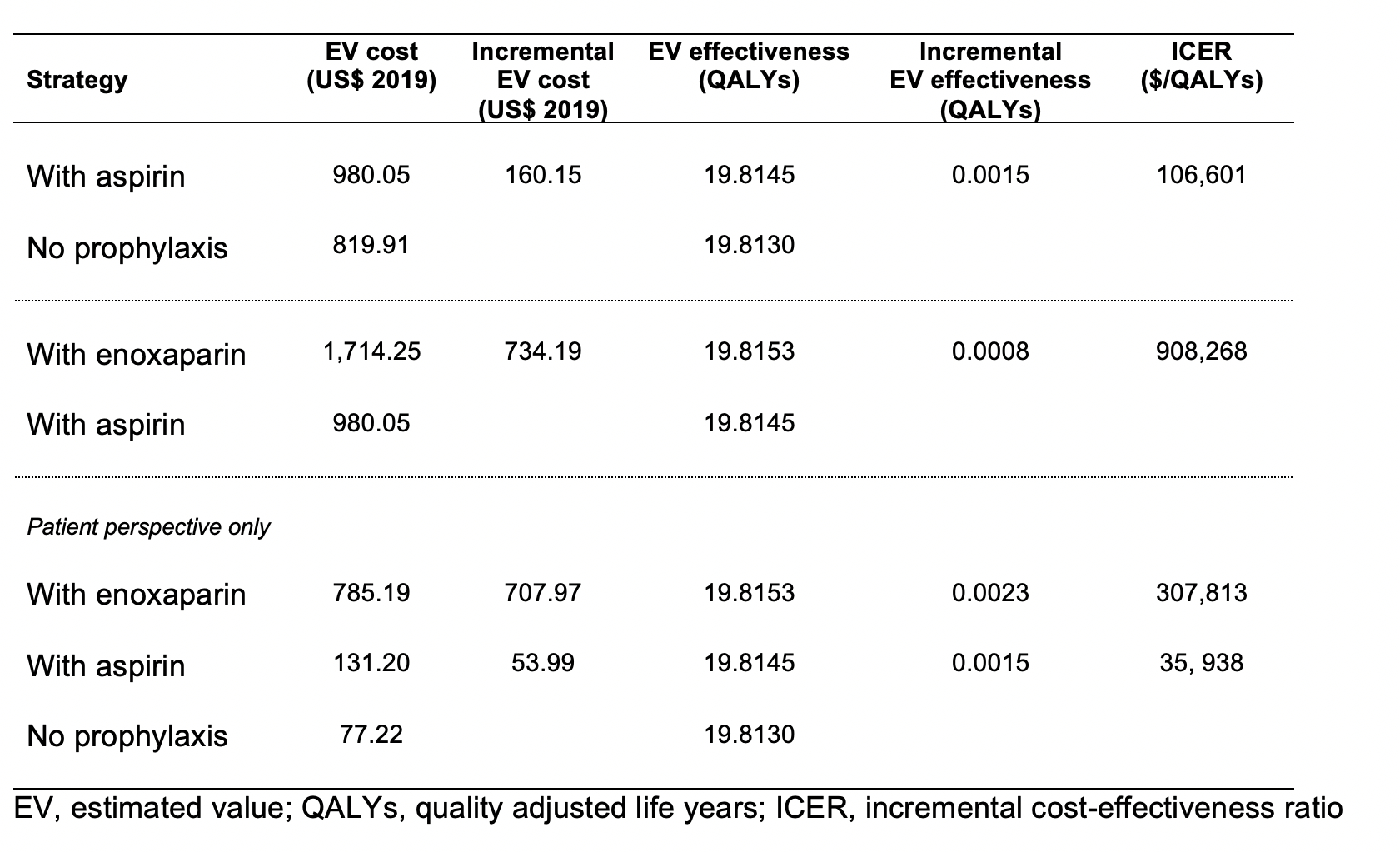
Table 1. Cost-effectiveness analysis of aspirin for extended venous thromboembolism prophylaxis following surgery for inflammatory bowel disease.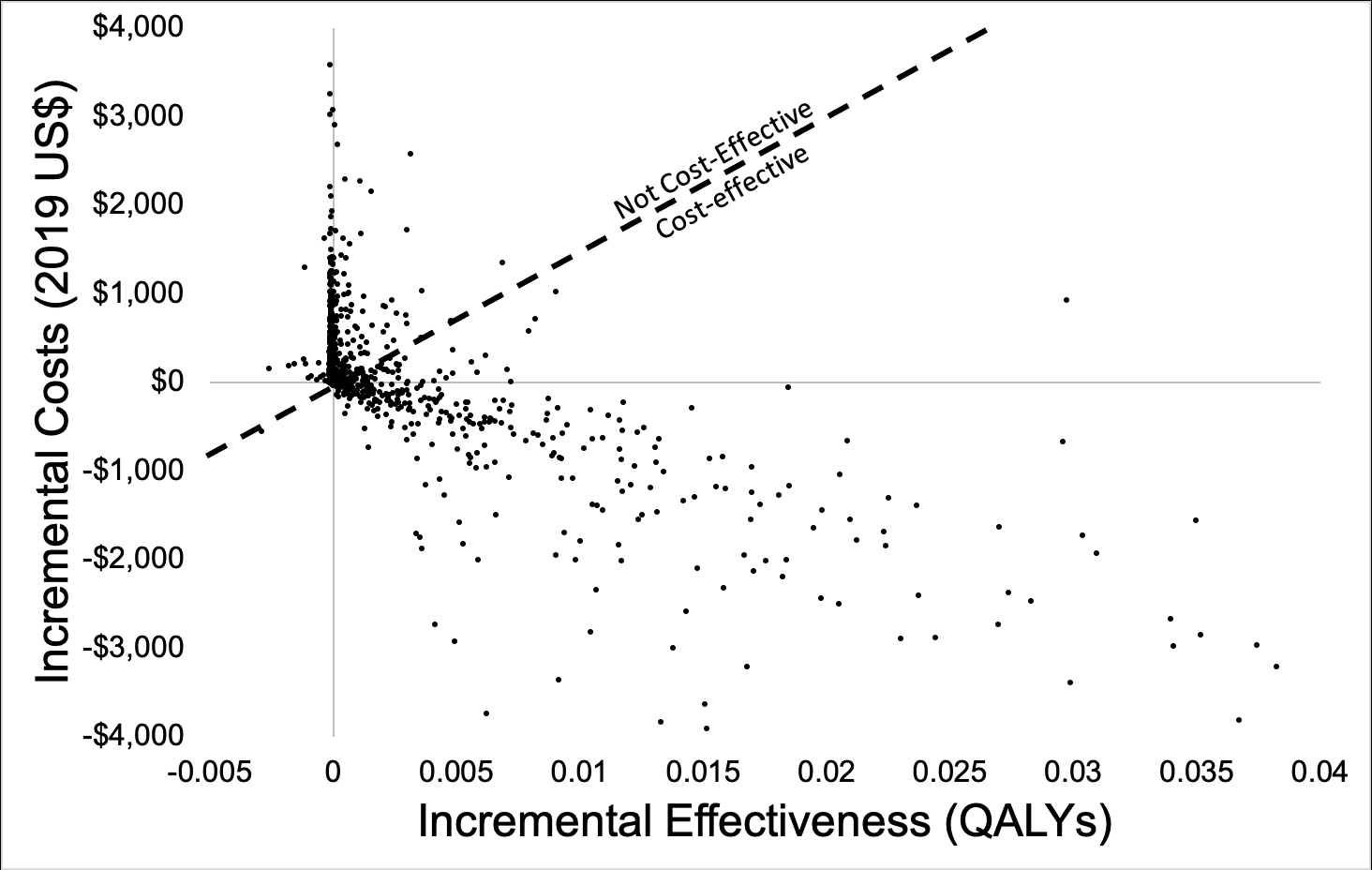
Figure 1. Cost-effectiveness plot of aspirin versus no prophylaxis for the post-discharge prevention of postoperative venous thromboembolism.
Back to 2021 Abstracts
