ASSOCIATION OF MEDICAID ELIGIBILITY WITH NON-ELECTIVE SURGERY, OUTCOMES, AND COSTS FOR COLON CANCER AMONG MEDICARE PATIENTS
Kathryn Taylor*2,1, Adrian Diaz3,1, Ushapoorna Nuliyalu1, Justin B. Dimick1, Hari Nathan1
1University of Michigan, Ann Arbor, MI; 2Stanford University, Stanford, CA; 3The Ohio State University, Columbus, OH
Introduction:
Increasing attention is being paid to the impact of social determinants of health on outcomes and utilization. Eligibility for Medicaid among Medicare patients (dually eligible, DE) has been used for social risk stratification. DE patients have been shown to have worse outcomes and require more post-discharge support after elective surgery. These patients may also present with more advanced disease, indicating an opportunity for intervention. This study aimed to assess the association of DE status with non-elective surgery for colon cancer and variation in outcomes and spending.
Methods:
Fee-for-service Medicare patients who underwent resection (not diversion alone) for colon cancer were identified using 100% Medicare claims data from 2014-2018. Patients were identified as DE versus Medicare alone (non-DE). These data were linked with county-level social vulnerability index (SVI), another measure of social risk. Multivariable regression was used to assess differences in non-elective surgery, ostomy creation, complications, readmissions, discharge disposition, and spending among DE patients. Outcomes were risk-adjusted for patient demographics, comorbidities, tumor location, hospital characteristics, and elective admission. The interaction between SVI and DE was explored.
Results:
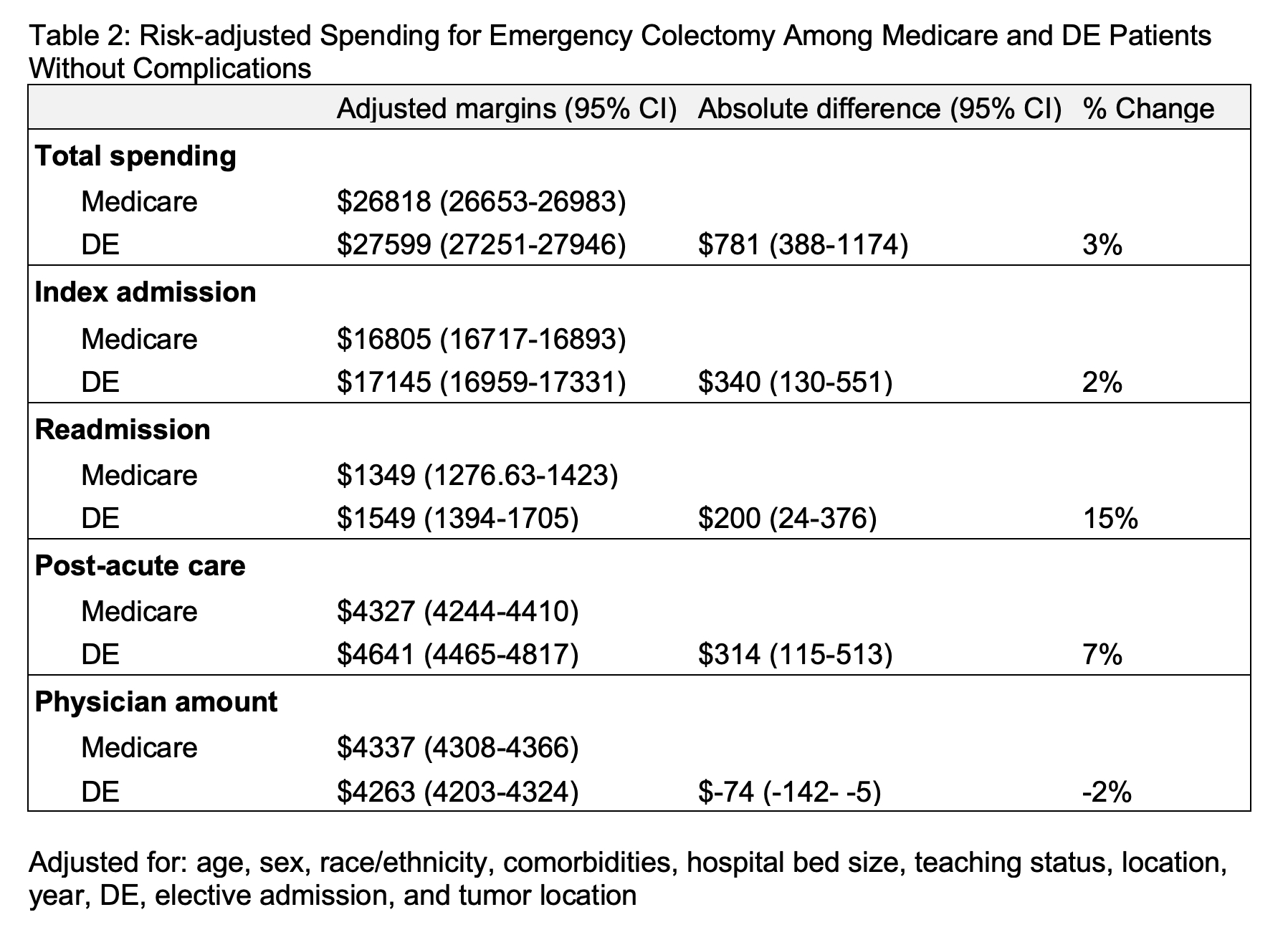
Of 146,041 Medicare patients included in the study, 24,795 (17%) were DE. The majority (65%) of colectomies were elective, and 7% of patients received an ostomy. More DE patients had a high SVI (score >75) compared to non-DE patients (34% vs 21%, p <0.001). DE vs non-DE patients had higher odds of undergoing non-elective colectomy (aOR 1.52, CI95% 1.47-1.57) and receiving an ostomy (aOR 1.26, CI95% 1.20-1.33), as well as higher rates of complications (Table 1). DE patients were less likely to be discharged home (aOR 0.48, 95% CI 0.47-0.50), even among those without complications and in both elective and non-elective groups. There was no significant interaction between DE and SVI, and aORs for DE did not vary significantly with adjustment for SVI. Among patients undergoing non-elective colectomy for cancer who did not experience complications (n=28,126, DE 20%), Medicare spending (total 30-day episode, index admission, readmission, and post-acute care) was significantly higher for DE patients (Table 2).
Conclusion:
DE patients were more likely to have non-elective colectomy, receive ostomies, and have complications compared to non-DE Medicare patients. DE patients, even when they had no complications, were less likely to be discharged home and incurred higher Medicare spending. These results indicate persistent associations of DE status with increased utilization independent of clinical presentation and outcomes. Providers should work to identify these at-risk patients and intervene prior to surgery in order to optimize outcomes and mitigate costs.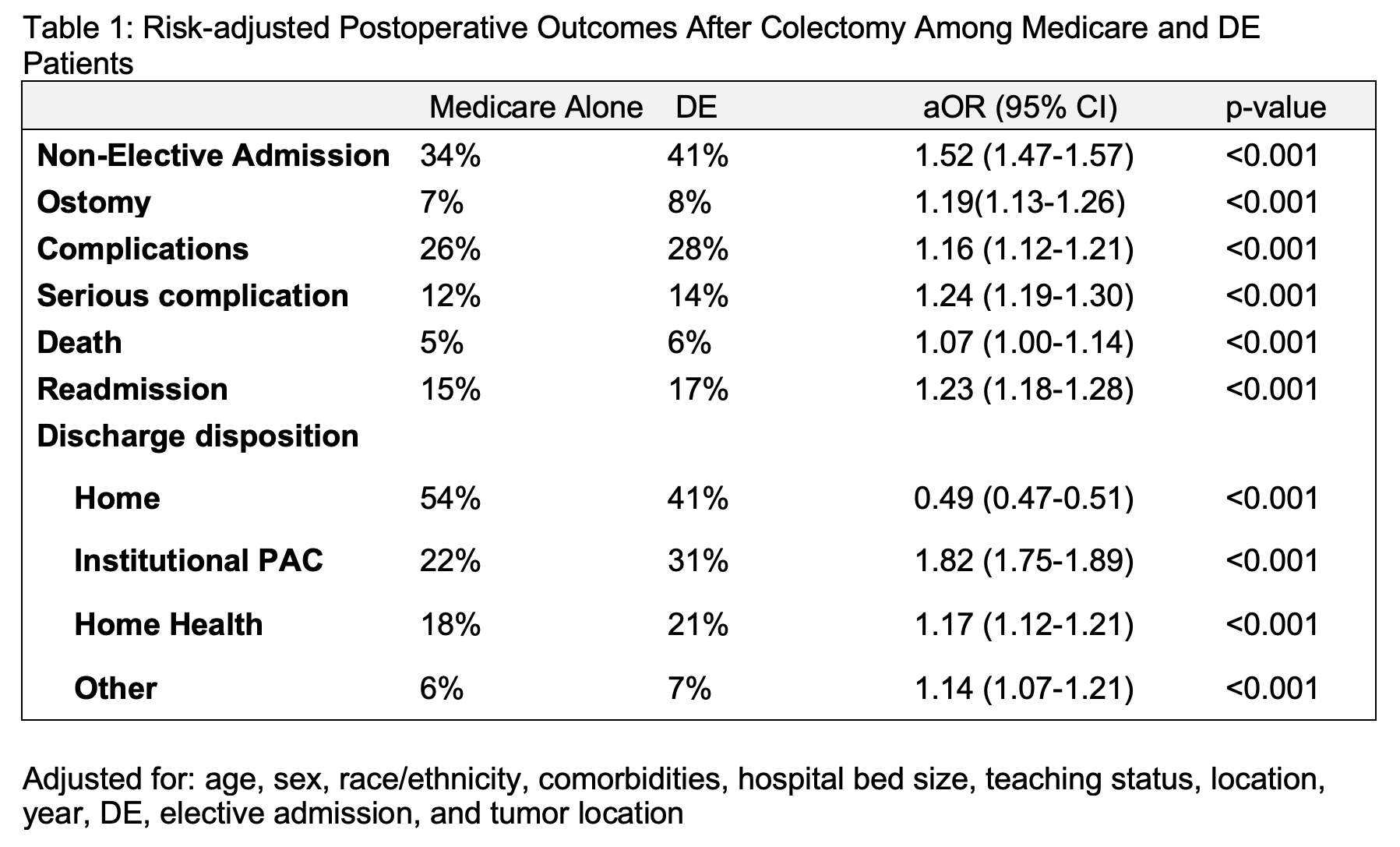
Back to 2021 Abstracts
