ASSESSMENT OF THE WEEKEND EFFECT IN INTESTINAL VOLVULUS BY HOSPITAL TEACHING STATUS: A POPULATION BASED STUDY
Amrita K. Chawla*, Faiz Afridi, Reza Hashemipour, Sushil Ahlawat
Rutgers New Jersey Medical School, Newark, NJ
Background
The weekend effect is a phenomenon that describes worse outcomes for admissions on the weekend relative to weekdays. Various explanatory theories exist including decreased staffing and delays in procedures on weekends. Despite its emergent nature, this effect has not been studied on intestinal volvulus (INV). This study aims to assess weekend versus weekday management of INV across all hospitals and by hospital teaching status.
Methods
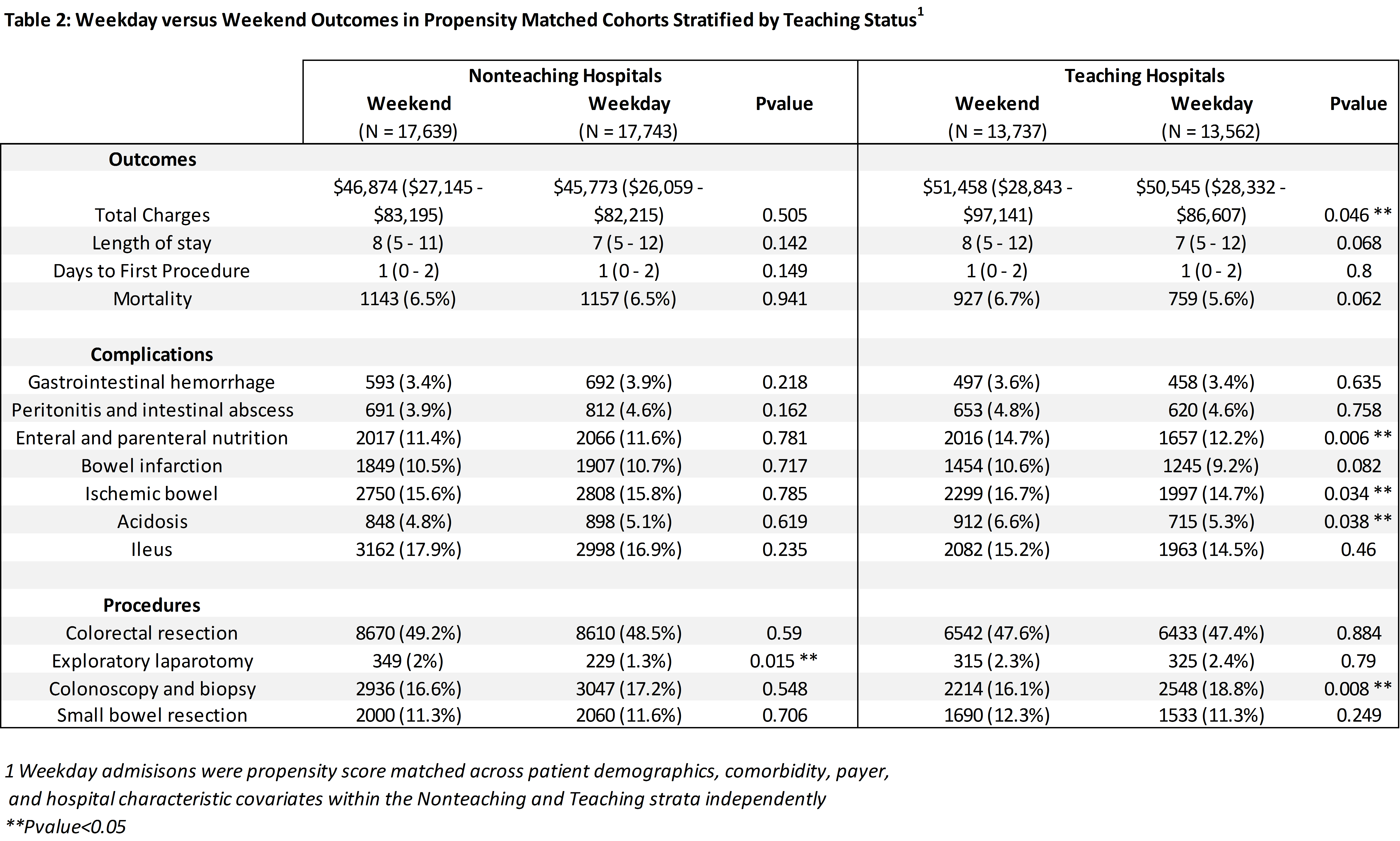
Patients with a non-pregnant status hospitalized for INV were identified from the 2001-2014 National Inpatient Sample (NIS) using ICD-9 codes. Baseline characteristics and outcomes were analyzed with Rao Scott chi squared and Kruskal-Wallis tests. Weekend admissions of INV were propensity matched with controls of weekday INV admissions across patient demographics, admission status, peritoneal adhesions, Elixhauser comorbidities, payer, and hospital characteristics. In order to assess differential weekend effects in teaching versus non-teaching hospitals, propensity matched analysis was conducted post-stratification of admissions by teaching status. Primary outcomes were length of stay (LOS), time to first procedure, total charges (inflation adjusted), and mortality. Secondary outcomes of post-operative complication rates were additionally assessed.
Results
186,132 cases of INV were identified of which 44,720 were admitted on the weekend. Pre-match, weekend admissions were older (71 vs 69, P<0.001) but had a similar frequency of comorbidities and prevalence of peritoneal adhesions [Table 1]. After matching, weekend and weekday admissions had similar mortality rates (6.6% vs 5.9%, P=0.1), median time to first procedure (1 vs 1 day, P=0.36), and LOS (8 vs 7 days, P=0.31). After stratification of hospitals by teaching status and matching within strata, mortality (6.5% vs 6.5%, P=0.94), median LOS, time to first procedure, and median charges were similar on weekends and weekdays at nonteaching hospitals [Table 2]. At teaching hospitals, weekend admissions were associated with higher charges ($51,458 vs $50,545, P=0.046), rates of ischemic bowel (16.7% vs 14.7%, P=0.034), acidosis (6.6% vs 5.3%, P=0.038), and enteral and parenteral nutrition (14.7% vs 12.2%, P=0.006). Teaching hospitals performed fewer colonoscopies and sigmoidoscopies (16.1% vs. 18.8%, P=0.008) on weekends but there was no difference at nonteaching hospitals.
Conclusions
Teaching hospitals perform fewer colonoscopies and sigmoidoscopies on weekends and are associated with a discernible weekend effect with higher complication rates and greater economic burden. These effects are not seen in non-teaching hospitals. Given INV is a medical emergency, review is needed to examine the drivers of this discrepancy to ensure uniform standard of care, adherence to best practices, and efficient resource utilization in teaching hospitals on weekends.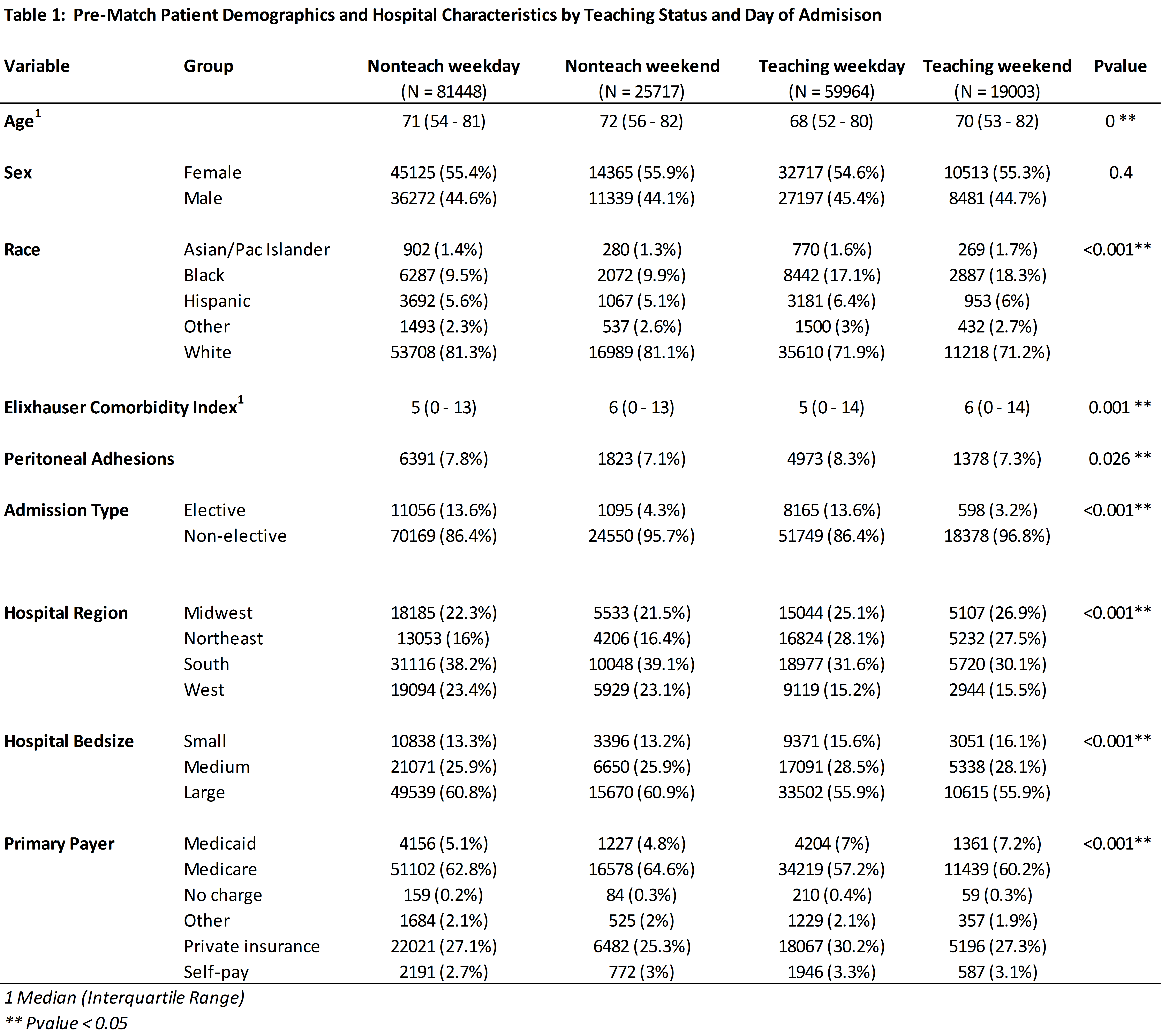
Back to 2021 Abstracts
