PANCREAS-SPARING DUODENECTOMY FOR ADVANCED DUODENAL POLYPOSIS IN PATIENTS WITH FAMILIAL ADENOMATOUS POLYPOSIS: SHORT AND LONG-TERM OUTCOMES
Arthur S. Aelvoet*, Barbara A. Bastiaansen, Olivier R. Busch, Evelien Dekker
Amsterdam UMC Locatie AMC, Amsterdam, North Holland, Netherlands
Background and Aim
Nearly all patients with familial adenomatous polyposis (FAP) develop duodenal adenomas and 4-10% duodenal cancer, warranting endoscopic surveillance. Extensive duodenal polyposis not amenable to endoscopic intervention may demand a surgical resection. In our center, a prophylactic pancreas-sparing duodenectomy (PSD) is offered for diffuse premalignant duodenal polyposis. We evaluated our 20-year experience with PSD.
Method
We performed a cohort study including FAP patients who underwent PSD between 2000 and 2020. Reconstruction with Billroth II anastomosis and short blind ending jejunal loop to the neo-papilla was performed to facilitate endoscopic surveillance, guided by the "neo-Spigelman" stage but not exceeding a 3 years interval. Data on short and long-term surgical outcomes and findings at surveillance endoscopies were evaluated.
Results
In total, 29 patients underwent PSD (15 men, median age 54). They had Spigelman stage III (n=6) or IV (n=23). No invasive cancers were found. Postoperative, 15 (52%) patients experienced a severe complication defined as Clavien-Dindo grade III or IV. Clinical relevant pancreatic fistula (grade B/C) occurred in 11 (38%) patients, gastro/duodeno-jejunostomy leakage in 4 (14%), delayed gastric emptying in 5 (17%) and 1 (3%) patient had severe acute pancreatitis. Median hospital stay was 14 days (IQR 9-29). No deaths occurred.
At long-term follow-up, 4 (14%) patients developed acute pancreatitis, 1 (3%) a new onset diabetes mellitus and 3 (10%) exocrine pancreatic insufficiency.
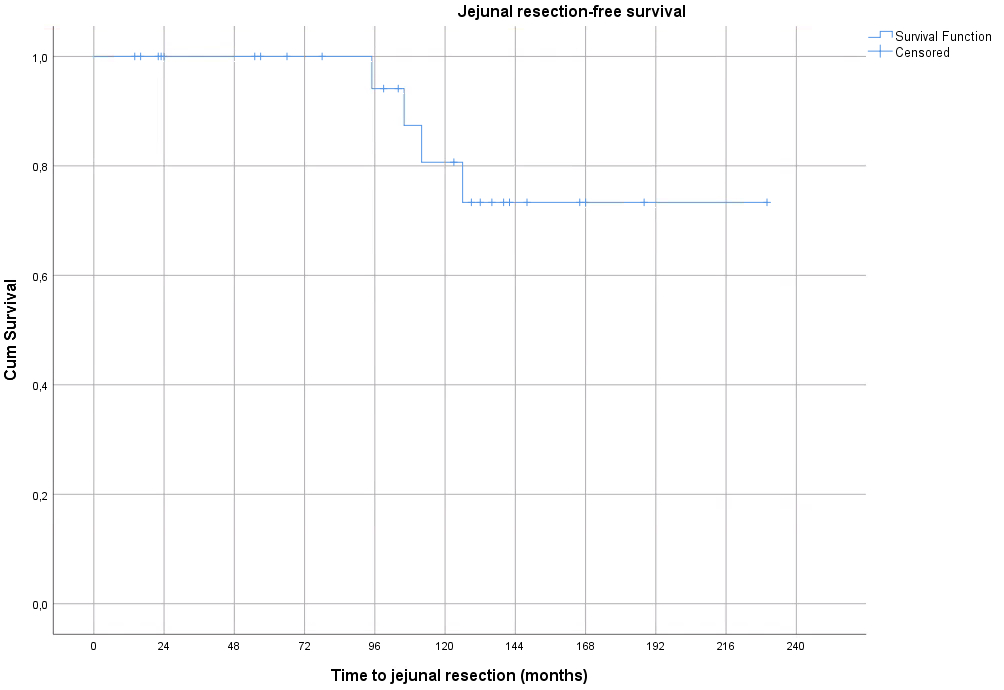
For surveillance, a total of 176 endoscopies were performed in 27 patients during a median follow-up of 119 months (IQR 55-148). Visualization of the end of the blind ending jejunal loop and neo-ampulla was documented in 25 (93%) and 22 (81%) of patients, respectively. In 22 (81%), one or more adenomas were detected in the jejunum. An advanced jejunal adenoma (defined as adenoma '‰¥10mm and/or HGD) was detected in 11 (41%) patients after a median of 44 months (IQR 14-19). Progression of jejunal polyposis resulted in neo-Spigelman stage IV in 7 (26%) patients after a median of 91 months (IQR 59-119). For 4 (15%) patients a surgical re-resection of the proximal jejunum was required for jejunal polyposis after a median of 109 months (IQR 98-123). No patients developed jejunal cancer.
Conclusions
PSD effectively prevents duodenal cancer in FAP patients with advanced duodenal polyposis. However, perioperative morbidity is substantial and most patients will have jejunal adenomas sometime at follow-up. With regular endoscopic surveillance, jejunal cancer can be prevented.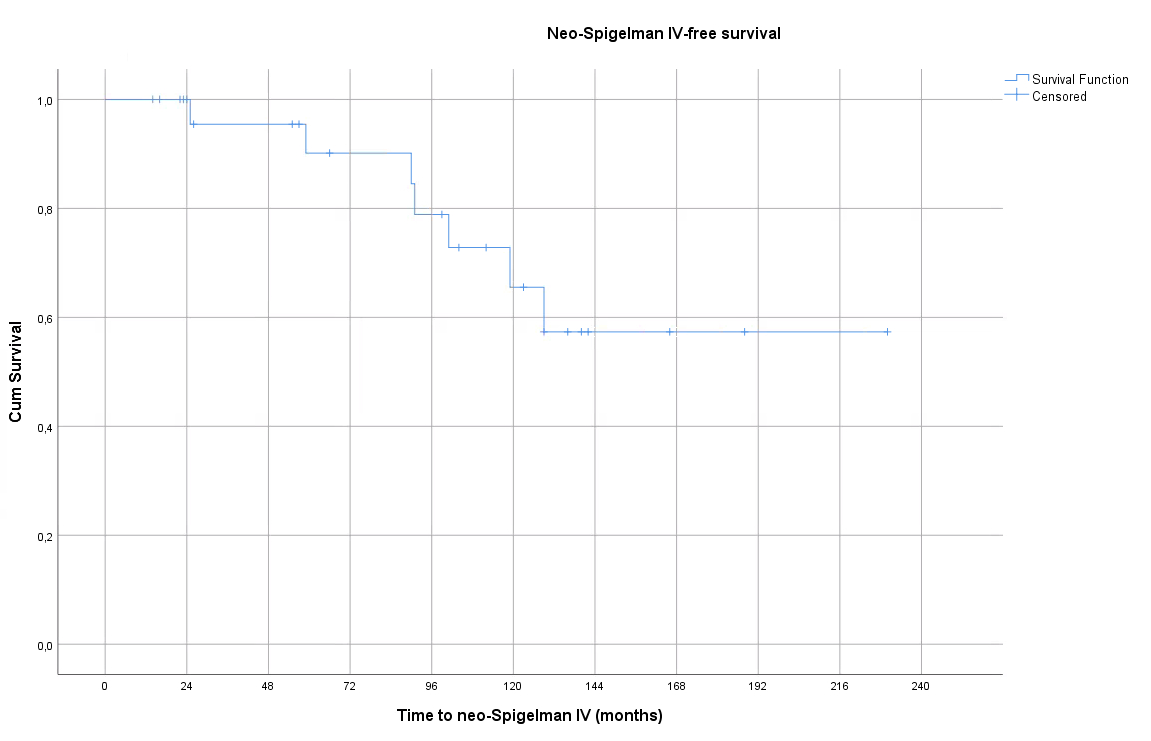
Back to 2021 Abstracts
