REASSESSING THE ROLE OF OPERATIVE INTERVENTION IN ELDERLY PATIENTS WITH NON-FUNCTIONAL PANCREATIC NEUROENDOCRINE TUMORS
Jonathan J. Hue*2, Kavin Sugumar2, Amr Mohamed2, J. Eva Selfridge2, David Bajor2, Joel Saltzman2, Jeffrey Hardacre2, John Ammori2, Luke Rothermel2, Jordan M. Winter2, Lee M. Ocuin1
1Surgery, Atrium Health, Concord, NC; 2University Hospitals, Cleveland, OH
Introduction: Pancreatic neuroendocrine tumors (pNETs) are rare and comprise 3% of pancreatic malignancies. Resection of locoregional disease is recommended but guidelines are conflicting. There is a paucity of data on the optimal management of pNETs in elderly patients.
Methods: The NCDB (2004-2016) was queried for patients >80 years old with localized pNETs. Patients were grouped based on non-operative or operative management. Demographics, postoperative outcomes, and survival were compared by univariable and multivariable analysis.
Results: A total of 591 patients were included in the analysis, of whom 202 underwent surgery and 389 did not undergo resection. Surgery was performed more commonly in younger patients (82 vs 83 years, p<0.001), at academic facilities (52.0 vs 43.4%, p=0.048), and for pancreatic body/tail tumors (80.7 vs 58.6%, p<0.001). There were no differences in tumor size (24 vs 25mm, p=0.628) or rate of Charlson-Deyo 0-1 patients (89.1% vs 89.7%) between patients who underwent surgery and those managed conservatively. On multivariable analysis, increasing age (OR 0.85, 95% CI 0.80-0.92) and pancreatic head tumors (OR 0.29, 95% CI 0.19-0.45) were associated with lower likelihood of surgery, whereas treatment at academic facilities (OR 1.46, 95% CI 1.01-2.12) was associated with a higher likelihood of surgery. The majority of resections were distal pancreatectomies (69.3%). The majority of resected tumors were grade 1 (79.2%), the overall node-positivity rate was 19.3%, and 7.4% of patients had positive resection margins. The median length of stay was 6 days, 30-day readmission was 9.4%, 30-day mortality was 4.0%, and 90-day mortality was 6.4%, which was higher for pancreatoduodenectomy than distal pancreatectomy (13.6% vs 5.1%, p=0.083). Patients who underwent surgery had longer survival than those who were managed non-operatively (80.8 vs 45.0 months, p<0.001; Figure 1), and this association was independent of tumor location (pancreatic head: 82.3 vs 36.1 months, p=0.009; pancreatic body/tail: 93.7 vs 53.4 months, p=0.001). On multivariable Cox proportional hazards analysis, operative intervention remained associated with longer survival (HR 0.69, 95% CI 0.50-0.95). In patients who underwent operative intervention, factors associated with improved overall survival included a Charlson-Deyo score of 0-1 (HR 0.21, 95% CI 0.08-0.58). Factors associated decreased overall survival included moderately differentiated (HR 3.29, 95% CI 1.19-9.14) or poorly differentiated tumors (HR 22.0, 95% CI 5.77-84.1), and positive lymph nodes (HR 3.63, 95% CI 1.60-8.24).
Conclusions: Resection of non-functional pNETs in elderly patients can be performed safely and is associated with improved survival compared to non-operative management. Surgery should be considered regardless of tumor location in appropriate operative candidates.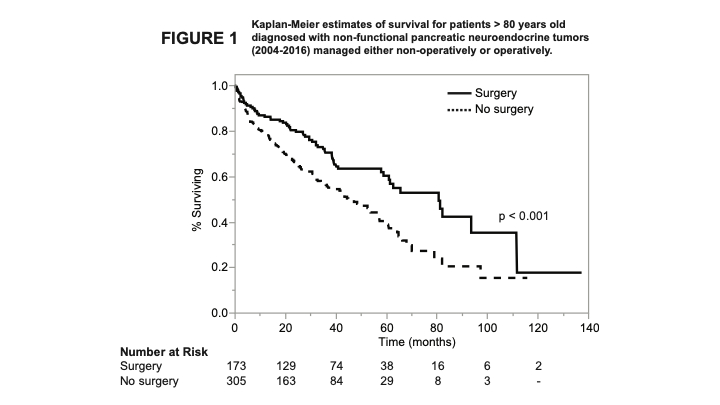
Kaplan-Meier estimates of survival for patients > 80 years old diagnosed with non-functional pancreatic neuroendocrine tumors (2004-2016) managed either non-operatively or operatively.
Back to 2021 Abstracts
