PANCREATICOJEJUNOSTOMY: INTRODUCING A NOVEL TECHNIQUE WITH LOW PANCREATIC FISTULA RATE
Maitham A. Moslim*1, Max D. Lefton1, Eileen A. O’Halloran1, Eric A. Ross1, Tamsin Board1, Andreas Karachristos2, Sanjay S. Reddy1
1Surgical Oncology, Fox Chase Cancer Center, Philadelphia, PA; 2University of South Florida, Tampa, FL
BACKGROUND: The pancreaticojejunostomy (PJ) anastomosis is the "Achilles heel" of the reconstructive phase of pancreatoduodenectomy (PD). Despite improvements in surgical techniques and perioperative care, clinically-relevant postoperative pancreatic fistula (CR-POPF) remains a significantly morbid complication after pancreatic resection. In this study we present our modification of the PJ dunking technique.
METHODS: This is a retrospective study of patients who underwent PD utilizing our novel modified dunking technique for PJ anastomosis. [Figure] A prospectively validated clinical fistula risk score (FRS) for POPF was utilized and calculated for each patient.1 Drain amylase was checked on postoperative day 3. The primary outcome was the occurrence of a CR-POPF which is defined as a grade B or C POPF. Thereafter, we identified two groups to compare: the CR-POPF group and the no CR-POPF group.
RESULTS: One hundred thirteen patients who underwent PD between 2012-2020 were included. CR-POPF was recorded in 7 patients (6.2%). The median age of diagnosis was 59.5 and 67.9 years for those with and without CR-POPF, respectively (p=0.38). There was no significant difference in gender distribution between both groups (p=0.7). The most common indication for PD was pancreatic ductal adenocarcinoma (n=71; 62.8%).
The two groups did not differ in terms of pathology (p=0.1), gland texture (p=0.08), pancreatic duct diameter (p=0.53), and intraoperative blood loss (p=0.47). All patients who developed CR-POPF had PD performed prior to 2017 (p=0.04). None of the CR-POPF group and 37.7% of the other group underwent neoadjuvant radiation (p=0.049).
There was no significant difference in fistula risk score (FRS) between both groups (p=0.072). The CR-POPF group had a median FRS of 3 and 4 for the procedures performed between 2012-2016 and 2017-2020, respectively (p=0.16). Although there were higher FRS in the latter (n=46), CR-POPF was not encountered.
CONCLUSIONS: In our cohort, the modified dunking technique for PJ yields a very low rate (6.2%) of CR-POPF. Although a learning curve is required to master this technique, the CR-POPF rate was brought down to zero in all cases performed in the last 4 years. We acknowledge the protective fibrosis and exocrine depleting effects of radiation; however, almost two thirds (65%) of patients had not received such treatment. We believe this is a safe and innovative technique that can be adapted and reproduced for both malignant and possibly benign pancreatic disease. A randomized clinical trial is warranted to validate and generalize this technique.
REFERENCE:
Miller BC, Christein JD, Behrman SW, et al. A multi-institutional external validation of the fistula risk score for pancreatoduodenectomy. J Gastrointest Surg. 2014;18(1):172-180.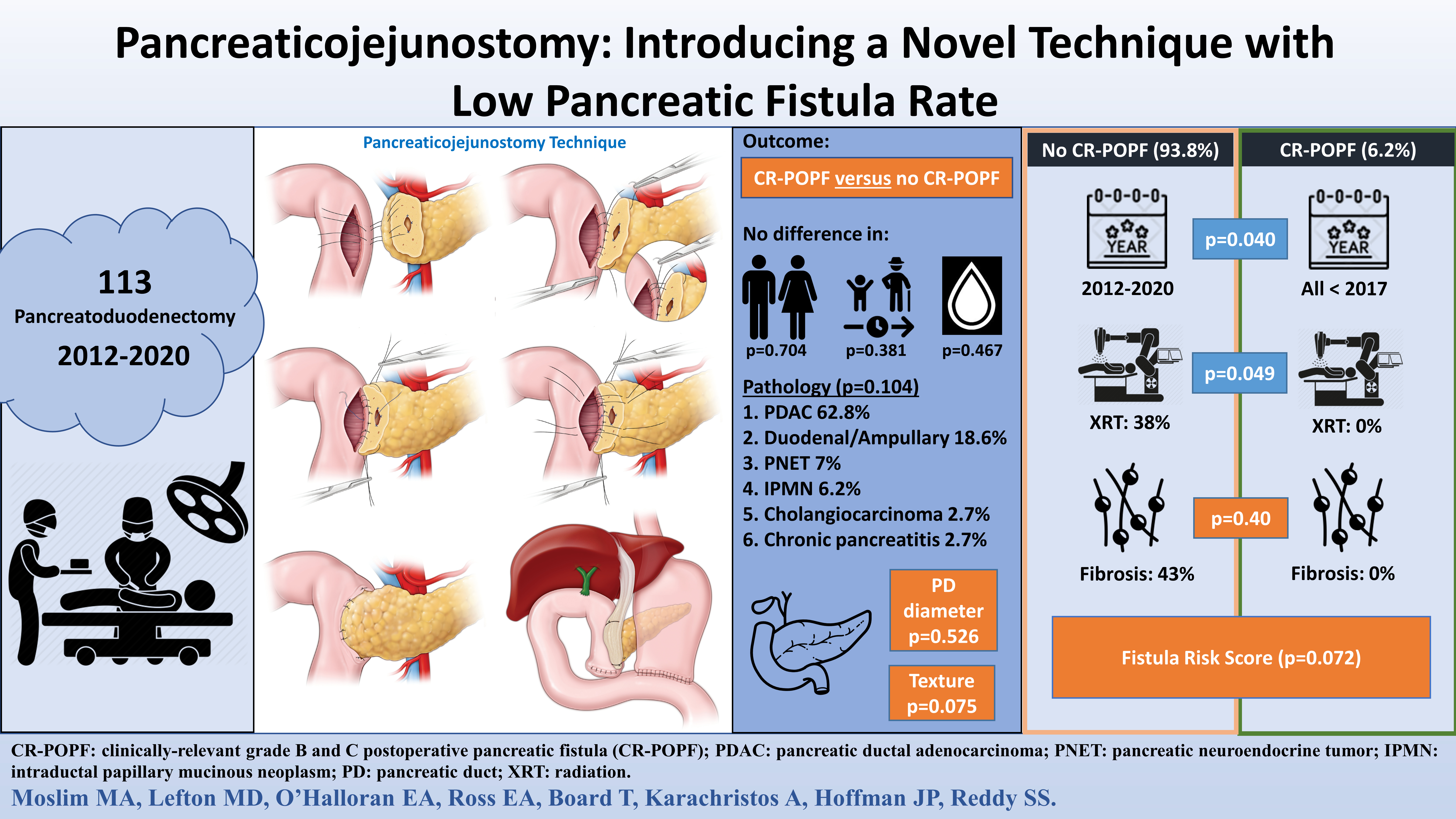
Back to 2021 Abstracts
