QUALITY OF LIFE OUTCOMES IMPROVE POSTOPERATIVELY IN PEDIATRIC PATIENTS UNDERGOING TOTAL PANCREATECTOMY WITH ISLET AUTOTRANSPLANTATION
Michael E. Johnston*1,2, Al-Faraaz Kassam1,2, Todd M. Jenkins2, Alexander R. Cortez1,2, Zishaan Farooqui1,2, David S. Vitale2, Tom K. Lin2, Maisam Abu-El-Haija2, Jaimie D. Nathan2
1Surgery, University of Cincinnati, Cincinnati, OH; 2Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Introduction: Pediatric patients with chronic pancreatitis (CP) have lower health-related quality of life (HRQOL) scores compared to the standard population. Total pancreatectomy with islet autotransplantation (TPIAT) is a surgical therapy offered after failure of medical and endoscopic intervention. We hypothesized that patients who underwent TPIAT have improved HRQOL postoperatively, regardless of post-operative adverse events or complications.
Methods: A retrospective review was performed of all TPIATs at a single institution from 2015-19. Patients completed a Short Form 36-Item Health Survey (SF-36) and Short Form 10 (SF-10) at enrollment and at regular intervals up to 24 months. Older children ('‰¥12 years old) completed the SF-36, a 36-item questionnaire while younger children (<12 years old) completed the SF-10 which is similar with reduced number of questions. Postoperative complications were defined according to the Clavien-Dindo scale and reviewed.
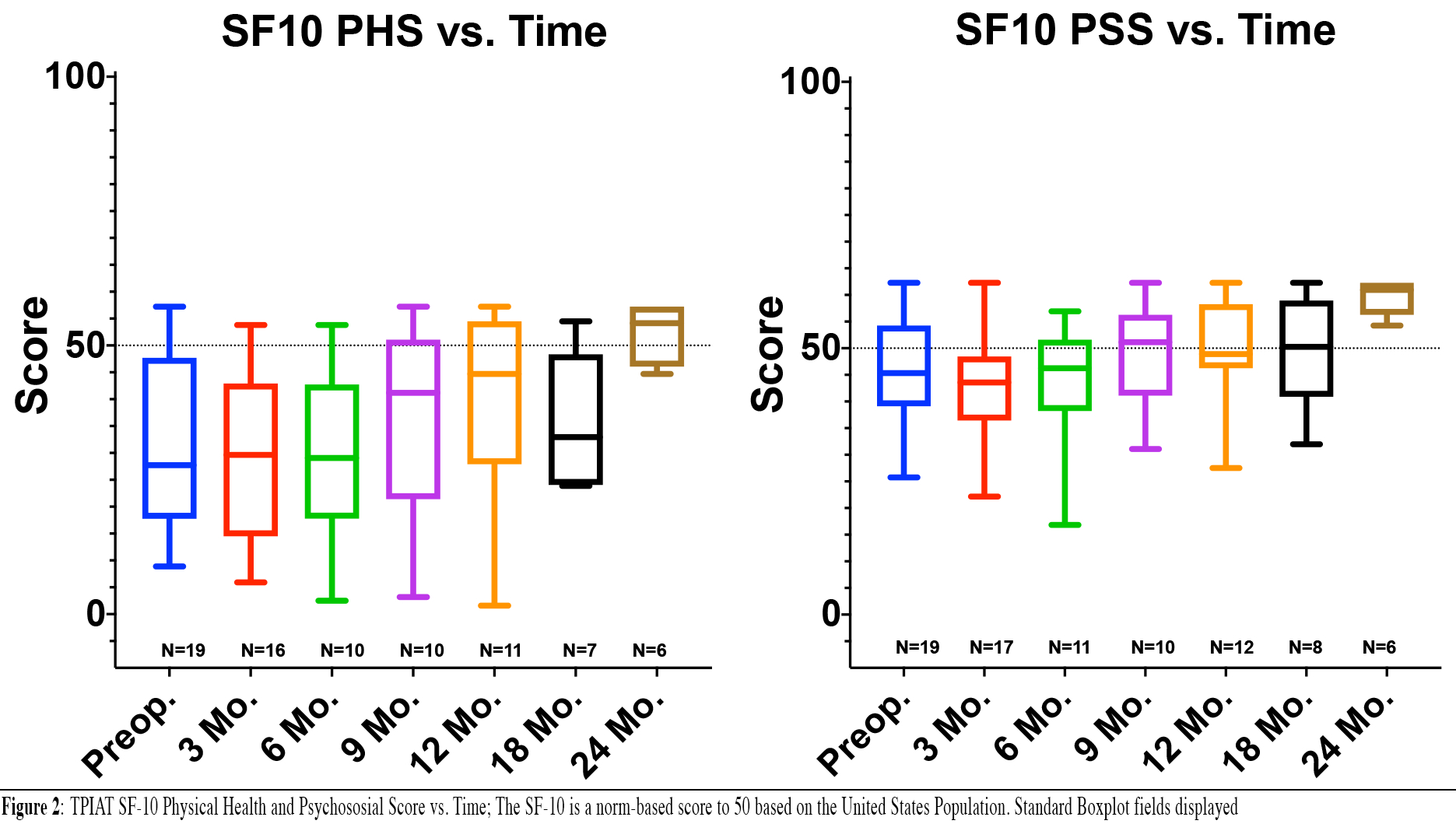
Results: Fifty-two patients underwent TPIAT with a median age 13 and 69.2% female. Thirty-two older patients and 19 younger patients completed the respective SF at enrollment.. Eleven patients (21.1%) had a Clavien-Dindo complication within 30 days, while four (7.7%) had a complication within one year requiring intervention. Four patients underwent re-operation within 30 days and 4 additional patients underwent operation later, within one year (7.7%). Three patients (5.8%) were readmitted within the first month after surgery while an additional 24 (46%) were readmitted later within the first year. Median postoperative follow-up was 30.1 months ('±21.8). Median total SF-36 preoperatively was 52.0 ('±33.5), physical score of 43.9 ('±39.3), and mental score of 61.2 ('±66.8). SF-36 Total, Physical, and Mental Health scores were significantly improved postoperatively compared to baseline at one year (p<0.001, <0.001, and 0.020 respectively) (Figure 1). Additionally, patients showed improvement in 6 of 8 SF-36 subcategories at one year of follow-up. SF-10 Physical Health Score and Psychosocial Scores improved over time but did not carry statistical significance (p=0.30 and 0.58 respectively) (Figure 2). Based on adjusted analyses at one year, no differences were noted in SF-36 total, physical, or mental score between those with and without complications (p>0.05 for each) or reoperations (p>0.05 for each). However, there was a significant inverse relationship between number of hospitalizations and physical score (p=0.012) and total score (p=0.017), but not with mental score (p=0.31).
Conclusion: TPIAT is an effective operation for debilitating CP or ARP in pediatric patients. This complex surgery carries potential morbidity; however, patients experience improvement in HRQOL scores despite postoperative complications. TPAIT should be highly considered in patients with life altering pancreatitis.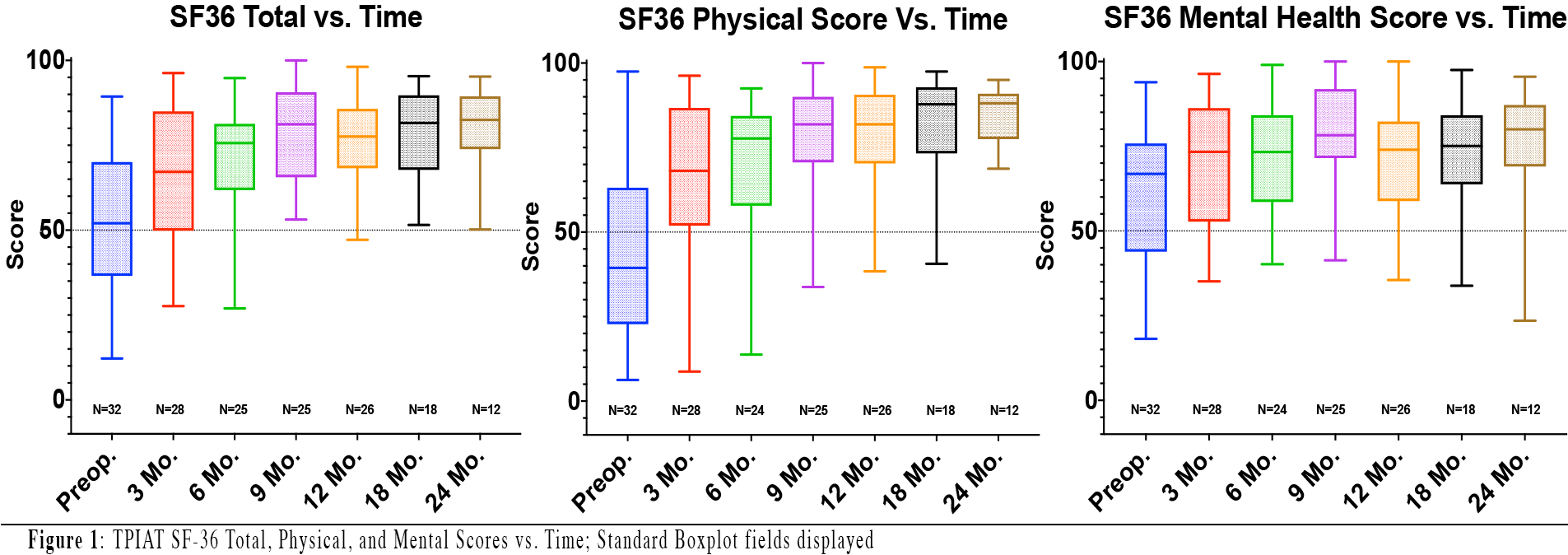
Back to 2021 Abstracts
