DECISION-MAKING AND PRACTICE HABITS FROM INTERNATIONAL MASTER SURGEONS REGARDING POSTOPERATIVE DRAIN MANAGEMENT AND TREATMENT OF PANCREATIC FISTULA FOLLOWING PANCREATODUODENECTOMY.
Fabio Casciani*1,2, Claudio Bassi2, Charles Vollmer1
1Surgery, Hospital of the University of Pennsylvania, Philadelphia, PA; 2University of Verona, Verona, Italy
Background
Postoperative management following pancreatoduodenectomy (PD) offers multiple decision-making points. Particularly, no consensus exists concerning drain management or therapeutic approaches in the case of pancreatic fistula development.
Methods
A questionnaire was sent to a select panel of international pancreatic surgery experts, recognized for their clinical and scientific authority. Their thought-processes and practice regarding drain management and treatment of clinically relevant pancreatic fistula (CR-POPF) were explored through checkbox questions, free-text responses, and situational clinical vignettes.
Results
60 surgeons from 22 countries, encompassing 73,304 pancreatic resections (median pancreatectomy/PD volume: 1200/705, median career duration: 22 years), completed the questionnaire. Drain fluid amylase (DFA) is the primary parameter these authorities consider for CR-POPF prediction (98%) and decision-making (95%) (Figure, top), yet only half routinely test serum amylase and 40% react to hyperamylasemia. POD3 is the timepoint when DFA is acquired most often (83%), with 45% sequentially assessing values on POD1 and POD3. 59% react primarily to actual DFA, while 41% rely on dynamics/kinetics. 77% feel fluid appearance is declarative of CR-POPF, whereas only 27% consider drain volume.
Among those managing drains based on POD1 DFA (53%), POD1 cutoffs commonly employed are 5000 U/L (50%) and 1000 U/L (19%). Early drain removal ('‰¤POD3) is employed by 88% when POD1 DFA is under their cutoff, while when DFA surpasses that value 65% would retest POD3 DFA, 58% keep the drains longer, and just a minority ('‰ˆ25%) would invoke additional tests/interventions. When faced with hypothetical clinical vignettes, experts are reluctant to apply early drain removal for high POD1 DFA or increasing DFA, and also show restraint when encountering high drain output or sinister fluid appearance.
When clinical deterioration occurs due to CR-POPF, experts unanimously opt for percutaneous drain placement as primary treatment, with 75% managing the patient in the ICU. Although many would not reoperate for a fistula, completion pancreatectomy is the most frequent approach endorsed when anastomotic disruption is ascertained (33%), yet with lack of consensus (Figure, bottom). Other operative strategies applied are wide drainage (27%) and pancreatic duct externalized stenting (20%), while most discourage re-constructing the anastomosis or occluding the pancreas.
Conclusion
Despite DFA measurement being established among experts, no agreement exists on timing and cutoffs employed for drain management. Percutaneous drainage is unanimously advocated as the first therapeutic option for CR-POPF, while contrasting strategies are employed when a re-operation is necessary. These insights indicate that optimal pathways of care following PD are variable and unresolved.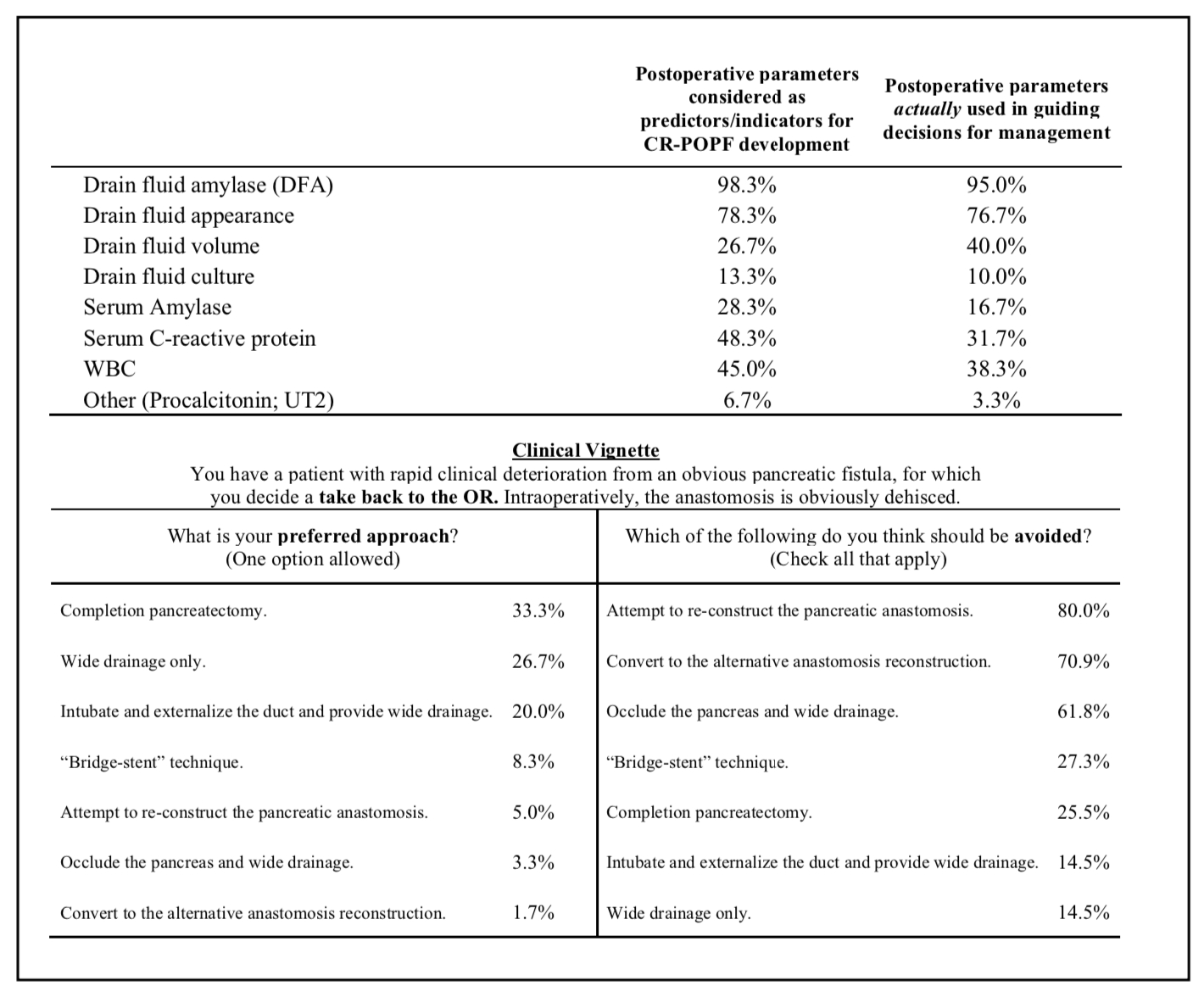
Practice habits and decision-making expressed by 60 international pancreatic surgery masters regarding parameters employed for pancreatic fistula prediction and management (top) and operative strategies considered in the case of reoperation for severe pancreatic fistula (bottom) following pancreatoduodenectomy.
Back to 2021 Abstracts
