THE INDEPENDENT IMPACT OF RACE, SOCIOECONOMIC STATUS, AND EDUCATION ON COMPLETION OF ADJUVANT THERAPY AFTER UPFRONT SURGICAL RESECTION FOR PANCREATIC CANCER
Roi Anteby*1,2,5, Carlos Férnandez-Del Castillo2,5, Cristina R. Ferrone2,5, Lawrence S. Blaszkowsky4, Theodore S. Hong3, Jennifer Y. Wo3, Keith D. Lillemoe2,5, Motaz Qadan2,5
1Harvard University T H Chan School of Public Health, Boston, MA; 2Massachusetts General Hospital Department of Surgery, Boston, MA; 3Department of Radiation Oncology, Massachusetts General Hospital, Harvard Medical School, Boston, MA; 4Department of Medicine, Division of Hematology-Oncology, Massachusetts General Hospital, Boston, MA; 5Newton-Wellesley Hospital, Newton, MA
Introduction
A multimodal approach of surgery and chemotherapy (with or without radiation) is the mainstay of therapy with curative-intent for resectable pancreatic ductal adenocarcinoma (PDAC). However, not all patients receive adjuvant therapy for various reasons including high postoperative morbidity, intolerance of side-effects, and limited access and resources for postoperative treatment. The aim of this study was to compare utilization trends and expected outcomes of surgery with adjuvant therapy compared with surgery alone.
Methods
The National Cancer Database was queried for patients diagnosed between 2006-2017 with stage I and II PDAC who underwent upfront resection. Multivariable regression was applied to identify factors associated with completion of adjuvant therapy. Kaplan-Meier analysis was used to examine survival.
Results
Of the 40,244 patients who met the inclusion criteria, 65.2% completed adjuvant therapy after resection while 34.8% were treated with upfront surgery alone. Receipt of adjuvant multimodal therapy increased from 57% in 2006 to 69% in 2017 (p<0.001).
Table 1 presents the adjusted odds ratios for receiving adjuvant therapy following upfront surgery for localized PDAC. Non-White race was associated with lower odds of receiving adjuvant therapy, when adjusting for age, comorbidity status, stage, readmission after surgery and other variables (Black or African American: OR 0.87, 95% 0.80-0.94; Hispanic, Latino or Spanish: OR 0.87, 95% 0.79-0.93, compared to White; p<0.001). Patients who resided in areas with the highest income quartile were more likely to complete adjuvant therapy than those from the lowest income quartile (OR 1.11, 95% 1.02-1.22; p=0.02); and patients who resided in areas with high education attainment were more likely to complete adjuvant therapy than those from low education attainment areas (OR 1.29, 95% 1.18-1.41; p<.001). Distance from hospital also played a role: the odds of receiving adjuvant therapy decreased by 46% (OR 0.54, 95% CI 0.5-0.57) for patients living more than 50 miles from the treating facility compared to <12.5 miles (p<.001).
The unadjusted median overall survival (OS) time was 17.8 months for surgery alone and 25.3 months for upfront surgery and adjuvant therapy. The overall 2-year and 5-year OS rates were 38.2% and 20.5% for surgery alone compared to 52.2% and 23.5% for surgery and adjuvant therapy (p<.001).
Conclusions
In this study examining utilization trends and expected outcomes of surgery with adjuvant therapy compared with surgery alone, there were wide socioeconomic disparities in the utilization of adjuvant therapy in patients who underwent upfront surgical resection for PDAC. This was independent of complications as represented by 30-day readmission. Completion of adjuvant therapy was associated with improved OS, highlighting the importance of multimodal treatment of PDAC.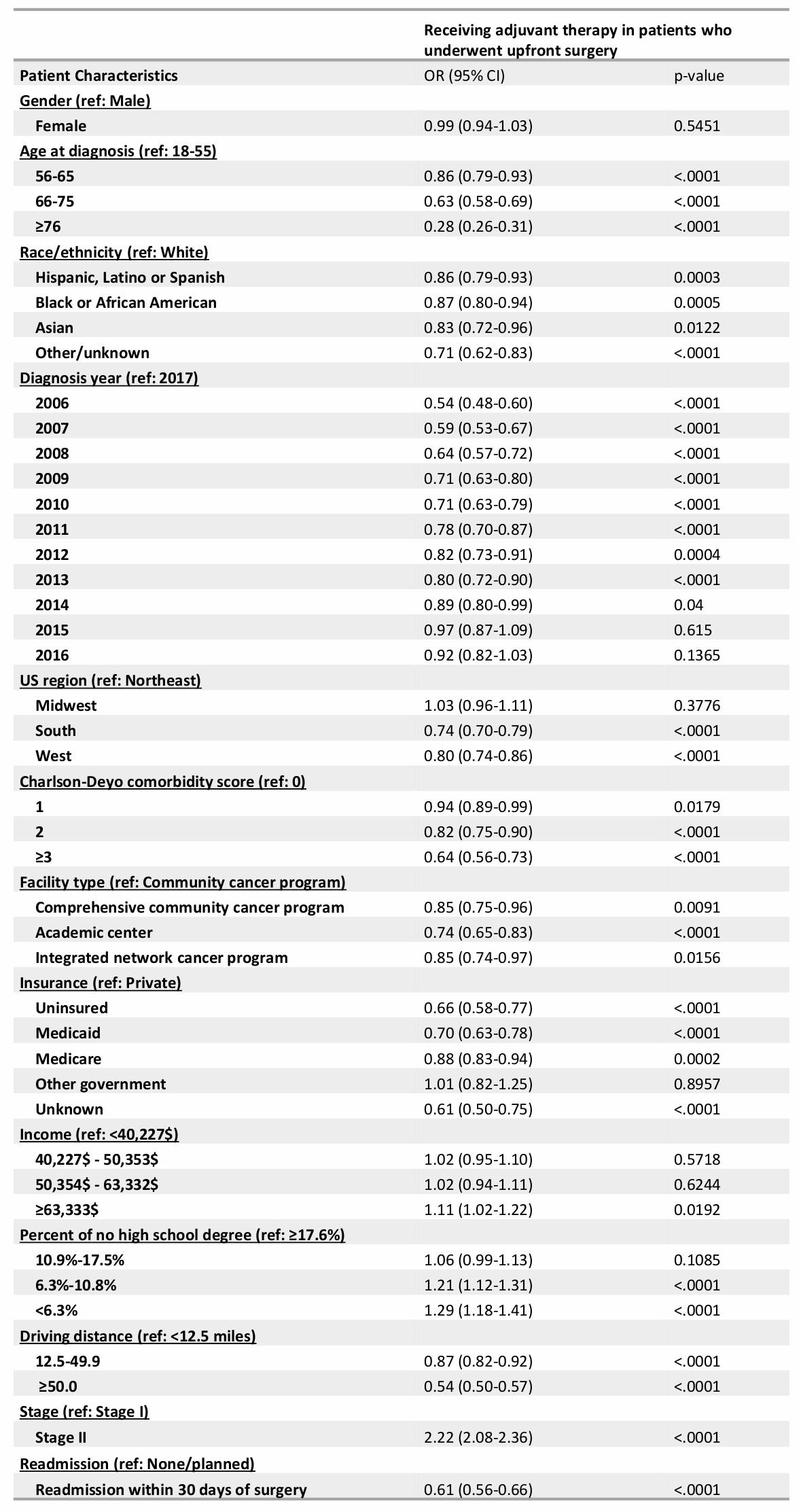
Back to 2021 Abstracts
