PROGNOSTIC IMPACT OF INTRAHEPATIC CHOLANGIOCARCINOMA TUMOR BURDEN FOLLOWING CURATIVE-INTENT RESECTION VARIES ACCORDING TO NODAL STATUS
Diamantis Tsilimigras1, Madison Hyer1, Adrian Diaz1, Alfredo Guglielmi2, Luca Aldrighetti3, Todd W. Bauer4, Matthew Weiss5, Sorin Alexandrescu6, George A. Poultsides7, Shishir K. Maithel8, Hugo P. Marques9, Guillaume Martel10, Carlo Pulitano11, Feng Shen12, Olivier Soubrane13, B. Groot Koerkamp14, Itaru Endo15, Timothy M. Pawlik*1
1Surgery, The Ohio State Wexner Medical Center, Columbus, OH; 2Universita degli Studi di Verona, Verona, Veneto, Italy; 3Ospedale San Raffaele Sede di San Raffaele Turro, Milano, Lombardia, Italy; 4University of Virginia, Charlottesville, VA; 5Northwell Health, Great Neck, NY; 6Institutul Clinic Fundeni, Bucuresti, Romania; 7Stanford University, Stanford, CA; 8Emory University, Atlanta, GA; 9Hospital Curry Cabral, Lisboa, Lisboa, Portugal; 10Ottawa Hospital, Ottawa, ON, Canada; 11university of sydney Department of surgery, Sydney, New South Wales, Australia; 12Eastern Hepatobiliary Surgery Hospital, Shanghai, China; 13Hopital Beaujon Service d'hepatologie, Clichy, Île-de-France, France; 14Erasmus Universiteit Rotterdam, Rotterdam, Zuid-Holland, Netherlands; 15Yokohama Shiritsu Daigaku Igakubu Daigakuin Igaku Kenkyuka, Yokohama, Kanagawa, Japan
Introduction: The prognostic impact of tumor burden (TB) relative to nodal status following resection of intrahepatic cholangiocarcinoma (ICC) remains ill-defined. We sought to assess whether ICC TB had a varied effect on outcomes among patients with N0, N1, and Nx disease.
Methods: Patients undergoing curative-intent resection of ICC between 2000-2017 were identified using a multi-institutional database. The impact of ICC TB [loge(tumor size) + number of lesions] on overall survival (OS) among patients who did (N0, N1) and did not (Nx) have lymphadenectomy was examined. The impact of ICC TB among Nx patients was also examined relative to preoperative imaging LN status (non-suspicious vs. suspicious).
Results: Among 1,097 patients who underwent curative-intent resection of ICC, 623 (56.8%) had low TB, 343 (31.3%) medium TB, and 131 (11.9%) high TB. LN status was N0, N1 and Nx in 29.3% (n=321), 19.7% (n=216) and 51.0% (n=560) of patients, respectively. In examining the entire cohort, ICC TB was associated with long-term prognosis (5-year OS; low-TB: 48.4% vs medium-TB: 29.8% vs high-TB: 17.3%; p<0.001) as was LN status (N0: 47.3% vs N1: 13.4% vs Nx: 43.3%; p<0.001). Among patients with N0 disease, lower ICC TB was strongly associated with improved OS (5-year OS; low-TB: 56.1% vs medium-TB: 41.3% vs high-TB: 27.8%; p=0.01); however, ICC TB failed to discriminate long-term prognosis among patients with N1 disease (5-year OS; low-TB: 17.9% vs medium-TB: 4.2% vs high-TB: 14.5%; p=0.44) (Figure). Among Nx patients, the impact of ICC TB varied according to the preoperative LN status. In particular, ICC TB was a strong predictor of outcomes among Nx patients with non-suspicious LN on preoperative imaging (3-year OS; low-TB: 66.9% vs medium-TB: 50.0% vs high-TB: 9.7%; p<0.001); in contrast, ICC TB failed to stratify prognosis among Nx patients with suspicious LN on imaging (3-year OS; low-TB: 52.9% vs medium-TB: 11.8% vs high-TB: 28.6%; p=0.10). On multivariable analysis, while ICC TB was associated with OS among patients with N0 disease (referent, low TB; medium TB: HR=1.54, 95%CI 1.11-2.14, p=0.01; high TB: HR=2.84, 95%CI 1.66-4.88; p<0.001), TB was not an independent predictor of survival among patients with N1 status (referent, low TB; medium TB: HR=1.12, 95%CI 0.71-1.76, p=0.62; high TB: HR=0.96, 95%CI 0.57-1.62; p=0.88).
Conclusion: While ICC TB was associated with survival among patients with N0 disease, ICC morphology was not predictive of long-term outcomes among patients with N1 disease. Lymphadenectomy during ICC resection is mandatory to define nodal status relative to tumor morphologic characteristics in order to stratify outcomes of ICC patients accurately.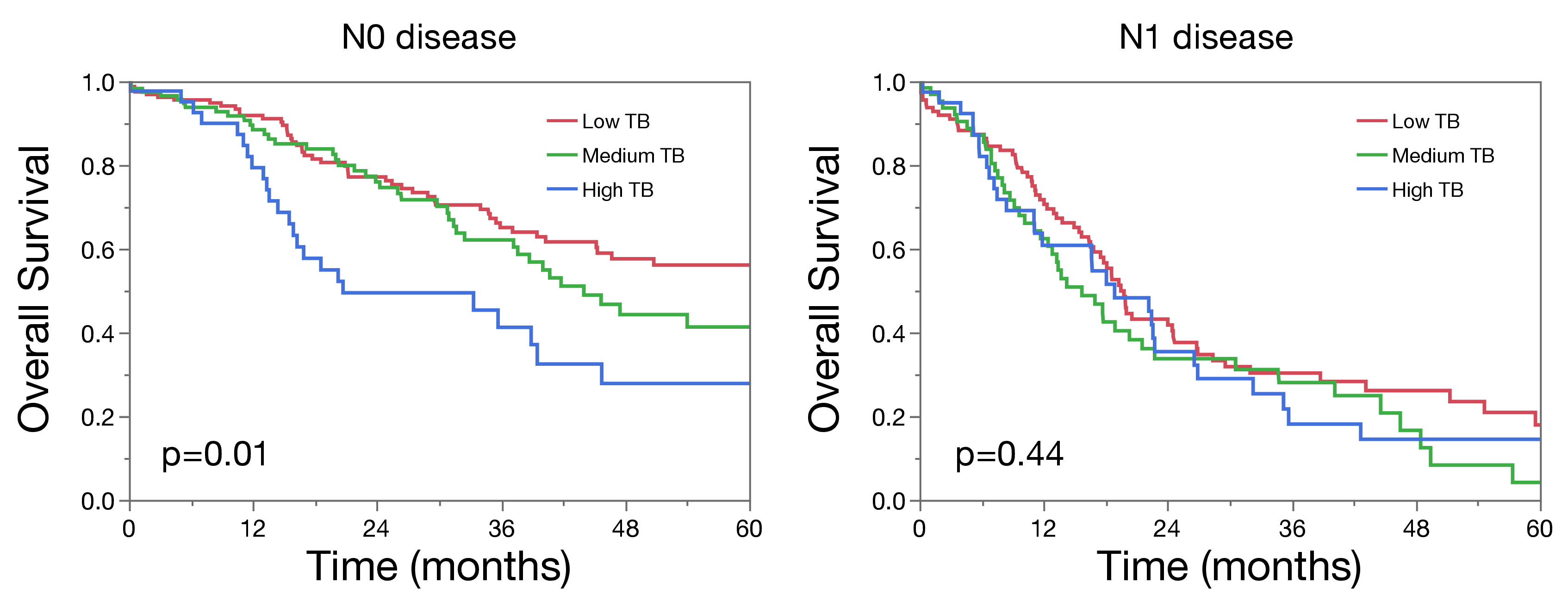
Back to 2021 Abstracts
