DO SURFACE MORPHOLOGY AND PIT PATTERN HAVE A ROLE IN PREDICTING CANCER FOR SESSILE COLON POLYPS IN NORTH AMERICA?
Ipek Sapci*, Madhusudhan R. Sanaka, Alexandra Aiello, Michael Valente, David Liska, Scott Steele, Emre Gorgun
Colorectal Surgery, Cleveland Clinic Foundation, Cleveland, OH
Background: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are widely utilized advanced endoscopic resection techniques in Eastern countries for premalignant and early malignant colorectal polyps. Correlation of submucosal invasion risk and endoscopic classifications based on lesion morphology and surface appearance has been described in the East, but not in North America. Our aim was to describe our experience with these advanced endoscopic resection techniques and investigate associations between the Paris classification, surface morphology, and Kudo pit pattern to submucosal invasion risk.
Methods: Consecutive EMR and ESD procedures performed on sessile polyps by a single colorectal surgeon between August 2017 and October 2018 were included in the study. Data were collected prospectively, and the following lesion characteristics were recorded: Paris classification (Is, IIa, IIb, IIc, III), surface features (granular, nongranular, mixed), and Kudo pit patterns (I-V). Lesion characteristics were observed by using a high definition colonoscope with narrow-band imaging when necessary. Multiple univariate analyses were conducted to compare characteristics across various groups, and Pearson's chi-square test, ANOVA, or the Kruskal-Wallis tests were used when appropriate. p-values <0.05 were considered statistically significant.
Results:151 lesions were removed using EMR or ESD. Mean age was 66.7 '± 10, and the median BMI was 29.0 [25.8, 34.4], and 53% of the patients were female. 138 sessile lesions were included in the final analysis. The successful resection rate was 95.7%, and the median injection volume to lift the lesion was 22.0[18, 34]ml. Median lesion size was 30 mm [25, 40], and the most common location was cecum (32%), followed by ascending colon (21%) and sigmoid colon (11.6%). On final pathology, 11 lesions had an invasive adenocarcinoma component (8%) and subsequently underwent oncological resections. Paris classification, surface morphology, and Kudo pit pattern correlation with submucosal invasion are in the table. Paris classification of IIa+c was associated with a higher submucosal invasion rate than the rest of the groups. Surface morphology based on granularity was not associated with submucosal invasion (p=0.39). Kudo pit pattern V was significantly associated with submucosal invasion (p<0.001), and 54.5% of lesions with submucosal invasion had type V in the final pathology.
Conclusion: Submucosal invasion risk can be predicted in the North American patient population by using pit patterns in sessile colorectal lesions by an experienced advanced endoscopist. Accuracy in cancer risk assessment may lead to better selection of the optimal advanced endoscopic resection technique such as EMR or ESD for high-risk lesions to ensure en-bloc and complete resection.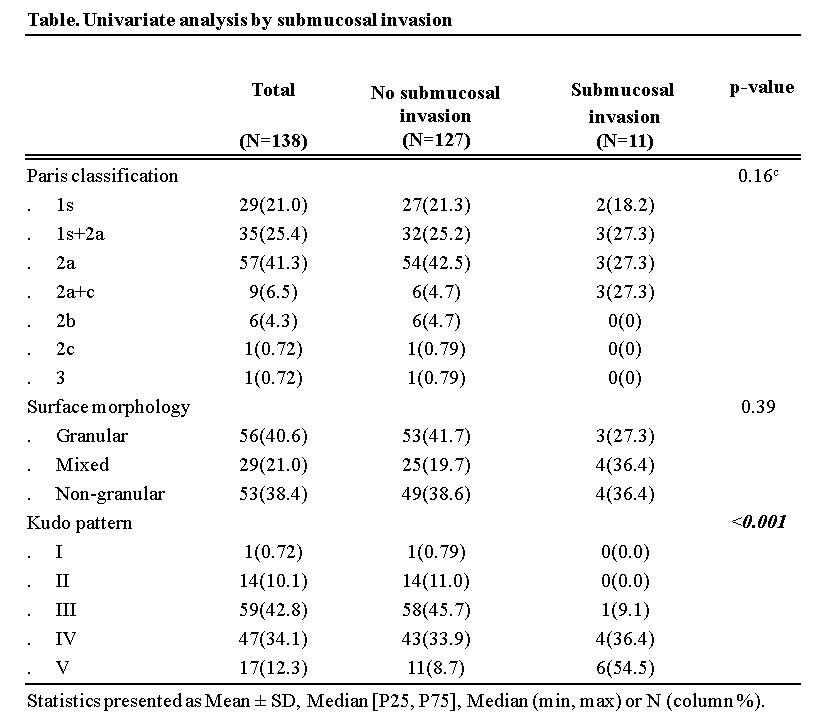
Back to 2021 Abstracts
