OSTOMY SURGERY FOR PATIENTS WITH LARGE BOWEL OBSTRUCTION IN THE MODERN ERA: A NATIONWIDE INPATIENT SAMPLE STUDY
Sudeep Banerjee*1, Mary Kwaan1, Yang Ren2, Yuqi Wu2, Sudha Xirasagar2
1University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 2University of South Carolina, Columbia, SC
Introduction: Management of large bowel obstruction has evolved over time. Although colostomy creation remains a mainstay of treatment, surgeons continue to seek alternatives to ostomy surgery (OS) such as resection with anastomosis or colon stent. In this study, we examined OS at the population level in the United States. Patients with emergency admissions and higher comorbidity profiles were expected to be more likely to have OS, but we hypothesized that socioeconomic determinants such as low-income level, lack of insurance, and public hospitals would be associated with higher rates of OS.
Methods: Adult patients with large bowel obstruction who underwent stoma or colorectal resection via ICD procedure codes were identified in the Nationwide Inpatient Sample (NIS), years 2010 to 2015. Etiology for obstruction was determined through ICD Diagnosis codes. Our primary outcome was OS. Concurrent colon resection and colon stent use was identified. Secondary outcomes included in-hospital death, length of stay (LOS) and discharge to facility. Multivariable regression analyses, adjusted for clinical covariates, socioeconomic and hospital factors were performed.
Results: Of 44,357 patients with large bowel obstruction, OS occurred in 35.8% and was more common patients with metastatic colorectal cancer (47.6%) and extracolonic cancer (49.7%). Older age (mean 64.4 vs 62.8 years), cancer diagnosis and high Charlson comorbidity were associated with OS, as was emergency admission (39.9%) and transfer from another facility (45.2%). Patients who underwent prior colon stent were more likely to undergo OS (58.7% vs 41.3%). Low income (36%), uninsured patients (39.9%) and Medicaid patients (41.4%) were more likely to receive an ostomy than patients with Medicare or private insurance (all p values <0.0001). With regard to structural and socioeconomic factors, after adjusted analysis, only hospital type and uninsured status were associated with ostomy surgery. (Table) Inpatient death was more common in those who had OS (6.8% vs 3.7%;p<0.0001) as was discharged to facility (28.6% vs 17%; p<0.0001). These patients also had a longer LOS by 2.4 days compared to patients who did not have OS. Using NIS weighted estimates, OS has increased in recent years.
Conclusion: Ostomy surgery remains frequently utilized for patients with large bowel obstruction, particularly in the emergent setting and among those with cancer. However over 50% of patients are managed without an ostomy, suggesting that further investigation into alternatives is important. Socioeconomic factors predispose to OS after adjusting for comorbidities and emergency status. Of note, temporizing measures with stents do not reduce rates of ostomy surgery if surgical intervention is eventually required. Patients who underwent OS had worse perioperative outcomes including higher inpatient mortality.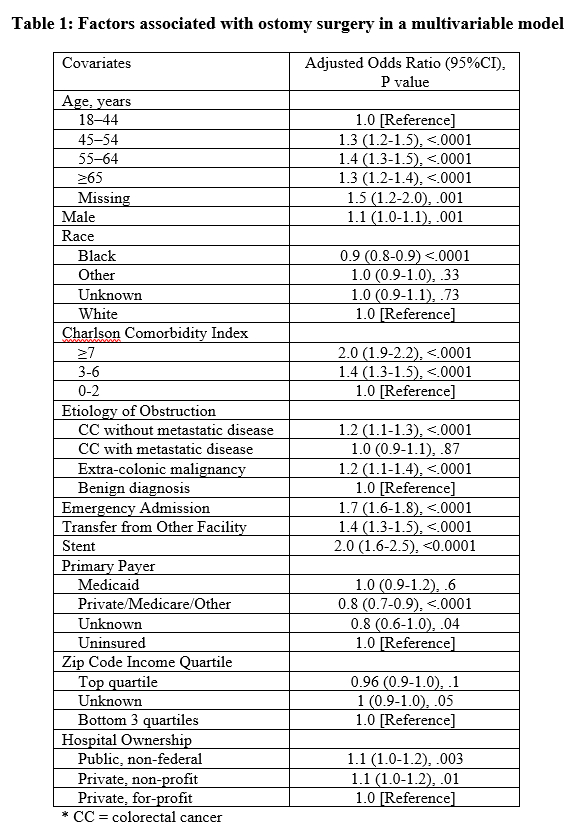
Factors associated with ostomy surgery in a multivariable model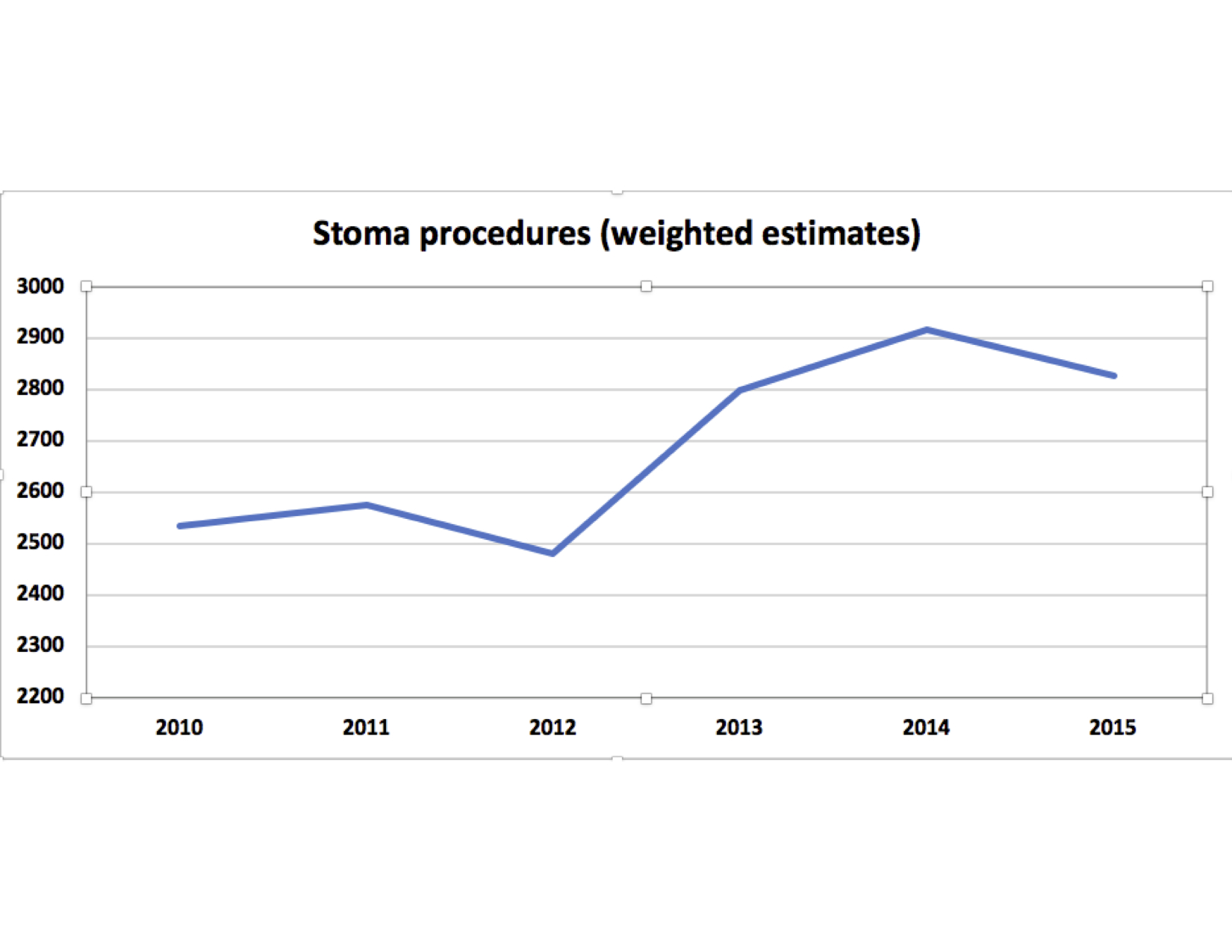
Back to 2021 Abstracts
