POPULATION-BASED LONGITUDINAL ASSESSMENT OF HOSPITALIZATIONS IN PATIENTS WITH METASTATIC COLORECTAL CANCER TO THE LIVER AND PERITONEUM
Michael P. O'Leary*, Philip H. Ituarte, Thuy B. Tran, Virginia Sun, Laleh G. Melstrom, Harold T. Huss, Isaac B. Paz, Yuman Fong, Mustafa Raoof
Surgery, City of Hope National Medical Center, Duarte, CA
OBJECTIVE: Patients with colorectal peritoneal metastases (CRPM) have worse overall survival than those with isolated colorectal liver metastases (CRLM). While the data on survival is robust, little is known about what that survival entails. Namely, the frequency of hospitalizations and need for intervention from the time of metastatic disease diagnoses to death. Therefore, we sought to better characterize the patient quality and burden of life by comparing admission time and frequency and interventions in those with CRPM versus CRLM starting from the time of diagnosis of metastatic disease.
METHODS: This was a retrospective study compiling patients with CRLM and CRPM diagnosed in the years 2000 to 2012 using the California Cancer Registry (CCR) in conjunction with data from the California Office of Statewide Health Planning and Development (OSHPD) inpatient database. The primary outcome was the number of hospitalizations per year of life after diagnosis of metastatic disease. Additional analyses included number of days hospitalized per year of life after diagnosis, overall and disease specific survival, requirement of gastrostomy tube placement, or parenteral nutrition. Groups were compared using Pearson Chi-Squared and Student's t-test. The Kaplan-Meier method and log-rank test were used to analyze disease specific and overall survival.
RESULTS: A total of 16,234 patients were included with 11,510 having CRLM and 4,724 having CRPM. The number of hospitalizations per year of life after diagnosis of metastatic disease was higher in those with CRPM (4.2 vs 3.2, p<0.001) as was the days hospitalized per year of life (66.2 vs 44.4, p = 0.002). Median overall survival (OS) in CRLM and CRPM were 9.9 and 7.5 months, respectively (p < 0.001, Figure 1). The need for gastrotomy tube placement was three times higher in those with CRPM (6.7% vs 2.2, p < 0.001). Parental nutritional support was required twice as often in those with CRPM (20.3% vs 10.5%, p < 0.001).
CONCLUSIONS: When compared to CRLM, patients with CRPM had worse OS and were in the hospital more often per year of life following their diagnosis of metastatic disease. Increased hospitalizations, requirement of procedures such as gastrostomy tube, and dependence on artificial nutrition makes this population particularly challenging to manage. This work should guide discussion with CRPM patients and more work should be done to describe the optimal treatment of these patients.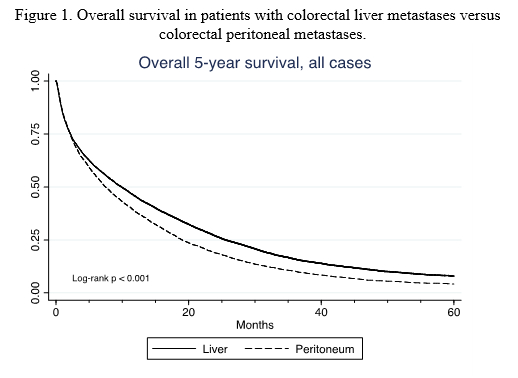
Back to 2021 Abstracts
