IMPACT OF PERIOPERATIVE NUTRITIONAL SUPPORT IN PATIENTS UNDERGOING MAJOR INFLAMMATORY BOWEL DISEASE SURGERY: A NATIONWIDE ANALYSIS
Andrew T. Weber*1, Minh Thu Nguyen2, Jenny S. Sauk1, Berkeley N. Limketkai1, Mary Kwaan3
1University of California Los Angeles Division of Digestive Diseases, Los Angeles, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 3University of California Los Angeles Section of Colon and Rectal Surgery, Los Angeles, CA
Background:
Patients with inflammatory bowel disease (IBD) frequently require surgical intervention for management of complicated or severe disease. IBD is often associated with protein-calorie malnutrition (PCM), a risk factor for adverse postoperative outcomes. This study aimed to assess the impact of perioperative nutritional support on relevant postoperative outcomes and complications.
Methods:
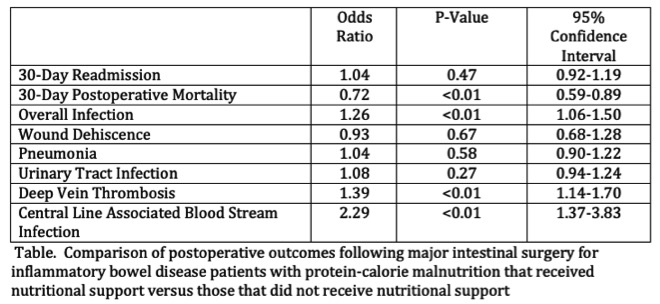
The Nationwide Readmissions Database (NRD) provides a large, nationally representative sample of patient-linked hospitalizations in the United States. We analyzed hospitalizations between the years 2010-2017 and identified patients with Crohn's disease or ulcerative colitis with concomitant PCM using International Classification of Diseases (ICD) codes. ICD procedure codes were further used to identify patients who underwent major intestinal surgery during the index hospitalization, as well as whether nutritional support (NS) was received via enteral (EN) and/or parenteral nutrition (PN). Postoperative outcomes of interest included 30-day readmission, infection, wound dehiscence, pneumonia, urinary tract infection (UTI), deep venous thrombosis (DVT), central line-associated bloodstream infection (CLABSI), and mortality. Using propensity score matching, patients who received NS were matched with patients who did not receive NS based on age, sex, IBD subtype, Charlson Comorbiditiy Index, elective admission status, patient income, expected insurance coverage, teaching hospital status, urban/rural hospital locality, and PCM severity. Logistic regression and Kaplan-Meier survival analysis were used to compare outcomes between the matched groups.
Results:
This study included 27665 patients with IBD and concomitant PCM who underwent major intestinal surgery; 14017 patients received NS (475 EN alone, 13098 PN alone, 444 both EN and PN) during the hospitalization and 13648 controls did not receive NS. NS was associated with lower odds of 30-day postoperative mortality (OR 0.72, p<0.01) but similar odds of 30-day readmission (OR 1.04, p=0.47) (Figure). NS was also associated with increased rates of overall infection (OR 1.26, p<0.01), CLABSI (OR 2.29, p<0.01), and DVT (OR 1.39, p<0.01). No significant differences were identified in rates of wound dehiscence, pneumonia, or UTI (Table).
Conclusions:
In our analysis of a large, nationwide database of patient-linked hospitalizations, utilization of NS in patients with IBD and PCM undergoing major intestinal surgery was associated with lower 30-day mortality. NS was, however, associated with increased infectious complications and DVT. Our findings indicate that perioperative NS has mortality benefit for high-risk IBD patients, particularly when balanced against risks of other postoperative complications.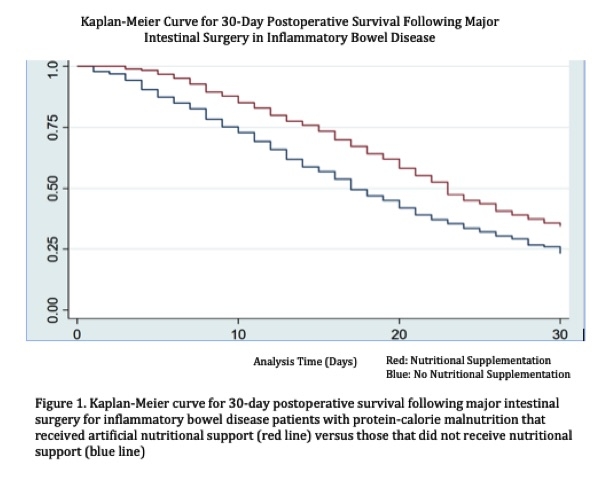
Back to 2021 Abstracts
