BLACK PATIENTS SUFFER SIGNIFICANTLY HIGHER ADVERSE EVENTS FROM BARIATRIC SURGERY DESPITE BETTER 30 DAY DECREASE IN BMI - AN ANALYSIS OF THE MBSAQIP DATA REGISTRY
Dilhana Badurdeen*, Abdellah Hedjoudje, Mohamad I. Itani, Atif Adam, Jad Farha, Lea Fayad, Michael Schweitzer, Vivek Kumbhari
Johns Hopkins Hospital, Baltimore, MD
Background: Racial disparities in bariatric surgery utilization have been noted, despite obesity affecting Black patients disproportionately. Our aim was to determine if Black patients have poor outcomes and adverse events regardless of baseline characteristics, type of surgery and surgical approach.
Methods: We identified patients undergoing RYGB and SG using the 2015-2019 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database. Univariate analyses were performed to determine predictors of serious morbidity and complications. Serious morbidity was defined as surgical site infection, wound dehiscence, ventilator dependence >48 hours, progressive or acute renal insufficiency (RI), cerebrovascular accidents, stroke, cardiac arrest, myocardial infarction (MI), bleeding requiring transfusion, pulmonary embolism (PE), sepsis, and septic shock. Variables significantly associated in univariate analysis were used in multivariate models.
Results: 107,449 Black and 341,380 White patients underwent RYGB or SG procedure between 2015-2019. Blacks were slightly younger 42.56'±10.96 vs 45.62'±12.28 years (p<0.001), and fewer patients were male, 13.1% vs 22.9% (p<0.001), respectively. At the time of surgery mean BMI in Blacks was 46.66'±8.34 kg/m2 vs 44.72'±7.61 kg/m2 (p<0.001) in Whites, and Black patients were less likely to be smokers 7.8% vs 8.9% (p<0.001). At 30 days, the mean decrease in BMI was 2.68'±2.63 vs 2.53'±2.54 (p<0.001), and 2.64'±2.48 vs 2.55'±2.43 (p<0.001) in Blacks vs Whites post RYGB and SG, respectively. Surgery characteristics such as utilization of laparoscopic, hand assisted, natural orifice transluminal endoscopic surgery (NOTES) versus single incision approach did not differ between Black vs White patients. Even though, robotic assisted surgery was utilized in 10.6% of Black patients compared to 8.9% of Whites, the use of robotic surgery did not predict serious morbidity or adverse events. Age, GERD, use of a mobility device, history of MI, previous cardiac surgery, HTN, history of deep venous thrombosis, RI, therapeutic anticoagulation, DM, chronic obstructive pulmonary disease, history of PE, sleep apnea, and use of chronic steroids at baseline predicted a higher incidence of serious morbidity and adverse events (Table 1). However, blacks have a 24% higher risk of serious morbidity and adverse events even after correcting for baseline characteristics, type of surgery and the use of a robot.
Conclusions: Weight loss at 30-days post-surgery is superior in Black patients. Despite better outcomes Black patients have a higher risk of serious morbidity and adverse events regardless of baseline comorbidities, type of surgery or surgery characteristics. Further studies are imperative to determine contributing factors, and to reduce healthcare disparity.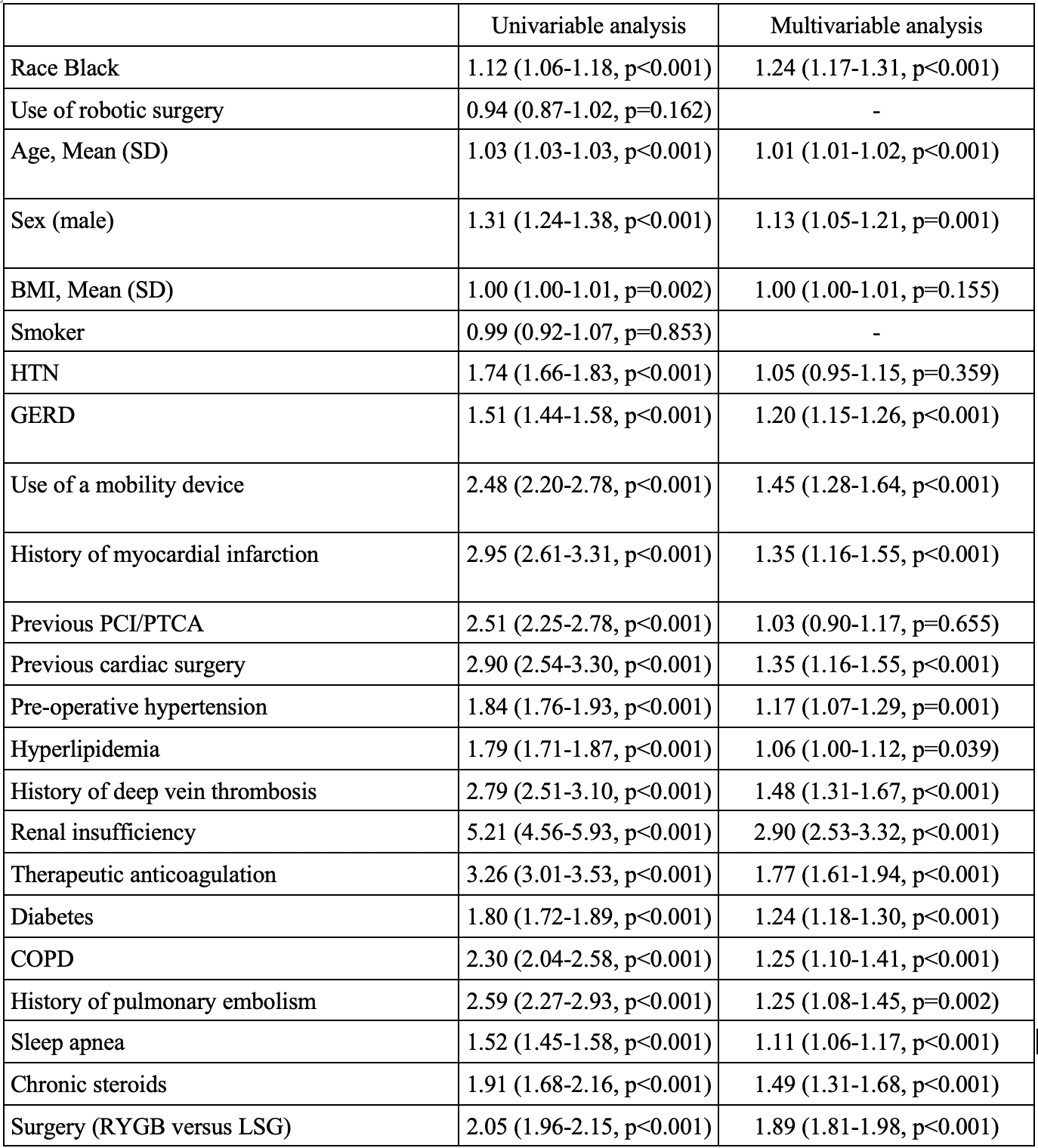
Table 1: Univariable and multivariable analysis of baseline characteristics, type of surgery and race contributing to serious morbidity and complications post-bariatric surgery.
Back to 2021 Abstracts
