NEITHER SURGICAL MARGIN STATUS NOR SOMATIC MUTATION PREDICTS LOCAL RECURRENCE AFTER R0-INTENT RESECTION FOR COLORECTAL LIVER METASTASES
Natalia Paez Arango*1, Yujiro Nishioka1, Yoshikuni Kawaguchi3, Federico Oppliger Boettcher1, Timothy E. Newhook1, Yun Shin Chun1, Thomas Aloia1, Ching-Wei D. Tzeng1, Hop Tran Cao1, Jeffrey Lee1, Timothy J. Vreeland2, Jean-Nicolas Vauthey1
1Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX; 2US Army Brooke Army Medical Center, Fort Sam Houston, TX; 3Hepato-Biliary-Pancreatic Surgery Division, Department of Surgery, the University of Tokyo, Bunkyo-ku, Tokyo, Japan
Objectives: Microscopic margin-negative (R0) resection has been traditionally thought to be required to minimize intrahepatic recurrences of colorectal liver metastases (CLM). However, the effect of somatic mutations such as RAS and surgical margin status on local and other intrahepatic recurrence remains unclear. We aimed to evaluate the association of surgical margins and somatic mutations with recurrence and oncologic outcomes.
Methods: CLM patients who underwent initial resection with R0 intent and genetic analysis of tumor tissue using next-generation sequencing during 2001-2018 were analyzed. First recurrence was classified as local recurrence (LR, recurrence at the margin of resection), other intrahepatic recurrence, or extrahepatic recurrence.
Results:
Of 552 patients analyzed, 415 (75%) had R0 resections (margin width '‰¥ 1.0 mm), and 525 (95%) had at least 1 somatic mutation. Thirty-eight patients (7%) had LR, and 265 patients (48%) had other intrahepatic recurrence. Recurrence site was not affected by the width of the surgical margin; 8% (11/137) of patients with margins <1.0 mm had LR, compared to 6% (8/141) of patients with margins >10 mm (p = 0.840) (Table). Common mutations were RAS/TP53 (184 patients), SMAD4 (70 patients), FBXW7 (40 patients), and BRAF (17 patients). RAS/TP53 co-mutation was associated with increased risk of postoperative recurrence overall (p < 0.001). However, the pattern of recurrence did not differ significantly by mutation type. Six percent (1/17) of patients with BRAF mutation, 8% (15/184) with RAS/TP53 co-mutation, 7% (5/70) with SMAD4 mutation, and 2% (1/40) with FBXW7 mutation had LR. (Figure). Cox proportional hazards model analysis showed that neither surgical margin status nor somatic mutation were associated with increased risk of local recurrence. LR occurred earlier than other intrahepatic recurrence (median 7.1 months vs. 10.3 months; p = 0.009). LR was associated with significantly worse overall survival than other intrahepatic recurrence (median 3.4 years vs. 5.4 years; p = 0.044).
Conclusions: Neither surgical margin width nor somatic mutation affects recurrence pattern including LR, although RAS/TP53 co-mutation is associated with increased recurrence risk overall. R0-intent resection was associated with a low rate of LR even if final pathological findings resulted in R1 resection. LR occurs sooner than other intrahepatic recurrence and is associated with worse survival.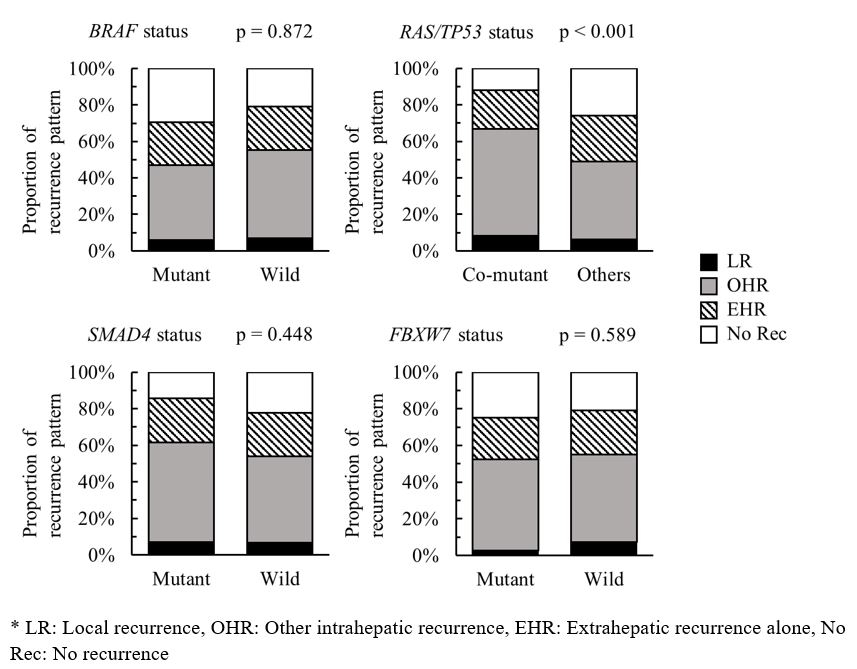
Figure. Patterns of recurrence stratified by mutation status*
Table. Patterns of recurrence stratified by margin status*
Back to 2021 Abstracts
