AMELIORATING EFFECTS AND MECHANISMS OF INTRA-OPERATIVE VAGAL NERVE STIMULATION ON POSTOPEARIVE RECOVERY AFTER SLEEVE GASTRECTOMY IN RATS
Ming Tian*1,2, Alimujiang Maisiyiti1,3, Payam Gharibani1, Jiande Chen1
1Johns Hopkins University, Baltimore, MD; 2Department of General Surgery, Dongzhimen Hospital Affiliated to Beijing University of Chinese Medicine, Beijing, China; 3Department of Minimally Invasive Surgery, Hernias and Abdominal Wall Surgery, People's Hospital of Xinjiang Uyghur Autonomous Region, Urumqi, China
Background: Sleeve gastrectomy is a common clinic operation for treating diabetes and obesity. The early recovery of gastrointestinal motility after surgery is an important influencing factor for shortening hospital stay and lowering the medical cost. The aim of this study was to explore the effects and mechanisms of intra-operative vagal nerve stimulation (iVNS) on promoting gastric motility after sleeve gastrectomy in rats.
Methods: Adult male Sprague-Dawley rats were randomly divided into two groups: sham-iVNS group (n=11) and iVNS group (n=12). All the rats received sleeve gastrectomy and were implanted electrodes on the chest for electrocardiogram (ECG) and gastric serosa for gastric pace-making activity. In iVNS group, iVNS was performed for 30 minutes during surgery. In sham-iVNS group, no stimulation was performed. The first drinking time, the first defecation time and the weight of daily stool were recorded after surgery. Autonomic functions were assessed from the spectral analysis of heart rate variability obtained from the ECG, and gastric pace-making activity (called slow waves) was recorded via the gastric serosal electrodes at 6h, 24h, 48h and 72h after surgery. Gastric empty was measured using a previously validated method at 72h after surgery.
Results: In comparison with sham-iVNS: 1) iVNS dramatically accelerated the first drinking time (41.17±8.13 vs. 89.09±15.05 min, P=0.01) and first defecation time (38.81±7.11 vs. 124.36±32.17 min, P=0.02); 2) iVNS increased the weight of stool in postoperative day (POD) 1 (2.66±0.35 vs. 1.45±0.25 g, P=0.01) and POD3 (3.49±0.61 vs. 1.56±0.26 g, P=0.01); 3) iVNS improved the gastric empty rate (79.4%±4.9% vs. 60.8%±5.7%, P<0.01) at 72h after surgery; iVNS increased the dominant frequency (5.36±0.62 vs. 4.57±0.47 cpm, P<0.01) and the percentage of normal gastric slow waves (47.18%±6.79% vs. 41.67%±4.58%, P=0.04) at 6h after surgery. 4) iVNS increased vagal activity and decreased sympathovagal ratio at 6h (vagal: 0.37±0.06 vs. 0.27± 0.07, P<0.01; sympathovagal ratio: 2.06±0.38 vs. 2.76±0.42, P<0.01) and 24h (vagal: 0.34±0.06 vs. 0.29±0.07, P=0.02; ratio: 1.96±0.37 vs. 2.44±0.45, P=0.01) after surgery.
Conclusions: Intra-operative VNS is effective in accelerating postsurgical recovery by enhancing gastric empty and gastric pace-making activity mediated via the autonomic mechanisms.
Fig.1 First drinking time, first defecation time, weight of stool and gastric empty rate. a iVNS accelerated the first drinking and first defecation time. b iVNS increased the weight of stool in POD1 and POD3. c iVNS improved the gastric empty rate at 72h after surgery. *P<0.05, **P<0.01 (paired t test)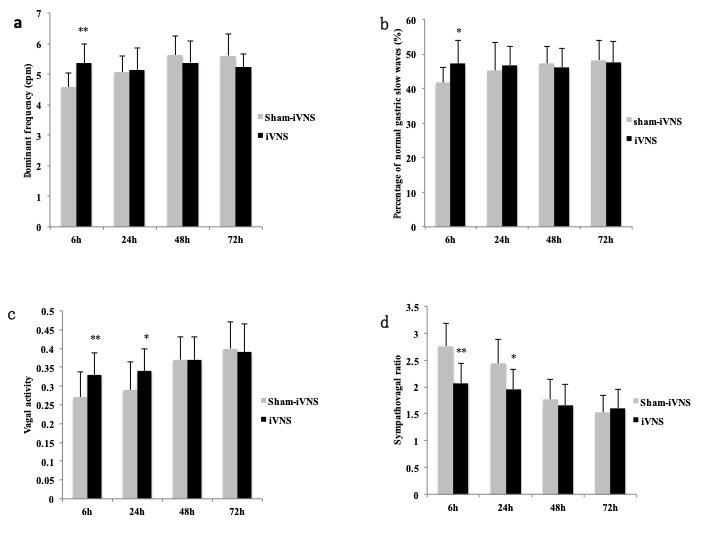
Fig.2 Gastric slow waves and heart rate variability. a iVNS increased the dominant frequency of gastric slow waves at 6h after surgery. b iVNS increased the percentage of normal gastric slow waves at 6h after surgery. c iVNS increased vagal activity at 6h and 24h after surgery. d iVNS decreased sympathovagal ratio at 6h and 24h after surgery. *P<0.05, **P<0.01 (paired t test)
Back to 2019 Posters




