CYTOREDUCTIVE SURGERY AND HYPERTHERMIC INTRAPERITONEAL CHEMOTHERAPY FOR OBESE PATIENTS: MORE CHALLENGING BUT WITH SIMILAR ONCOLOGICAL BENEFIT.
Eliahu Y. Bekhor*1,2, Brianne Sullivan1, Daniel Solomon1,2, Natasha DeNicola1, Margaret Hofstedt1, Eric Pletcher3, Matthew Carpiniello3, Jacquelyn Carr1, Nathan M. Bolton1, Benjamin Golas1, Deepa Magge1, Daniel Labow1, Umut Sarpel1
1Division of Surgical Oncology, Icahn School of Medicine at Mount Sinai, New York, NY; 2Department of surgery, Rabin medical center, Petach Tikva, Israel; 3Department of surgery, Icahn School of Medicine at Mount Sinai, New York, NY
Background: Obesity is a pandemic in the western world with over 40% of the US population with BMI>30kgm2. High BMI to can make surgical procedures more challenging and increase postoperative complications. We aimed to describe the clinical and oncological outcomes for obese patients with Peritoneal carcinomatosis (PC) who underwent Cytoreductive Surgery.
Methods: Patients with PC who underwent CRS/HIPEC between 2007 and 2018 at our institution were included from a prospectively maintained database. Clinical and oncological outcomes of obese patients were compared to that of normal weight patients.
Results: Overall, 410 CRS/HIPEC procedures were recorded at our institution; among these, 307 patients had 18.5<BMI<30, 87 patients had BMI>30, and 16 patients had BMI of <18.5. Gender, age and neoadjuvant therapy were comparable (p=NS). Obese patients had significantly higher ASA class (mean, 2.8 vs 3.0 p=0.006) and more challenging operations, as reflected by longer operative course (minutes, 318 vs 344 p=0.05), higher estimated blood loss (milliliters, 464 vs 680, p=0.025), and less laparoscopic operations (%, 14 vs 6, p=0.05), but with similar optimal cytoreduction (%, 94 vs. 99 p=0.09).
Post-operative course was similar (p=NS) in terms of 30 days Clavien IIIIV, 30 days mortality, ICU admission, and overall length of hospital stay.
At median follow-up of 30 months, there was no significant difference between recurrence rate (61% vs. 63%), disease-free survival (mean months, 18.3 vs. 15.3), and overall survival (mean months, 30.1 vs. 30.4).
Conclusions: Obese patients with PC have more comorbidities, longer and more challenging operations, and yet, benefit from CRSHIPEC with similar clinical and oncological results as normal weight patients, Thus, obesity should not be a contraindication to CRS/HIPEC in patients who are otherwise candidates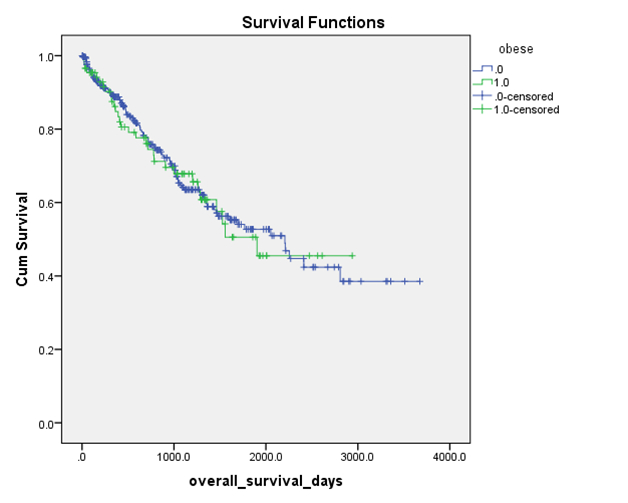
Back to 2019 Posters




