NINETY-DAY READMISSIONS FOLLOWING ROUX-EN-Y GASTRIC BYPASS SURGERY: TRENDS, CAUSES, AND RISK STRATIFICATION TOOL
Shashank Sarvepalli*1, Zubin Arora2, Madhusudhan R. Sanaka1, Gautam N. Mankaney1
1Gastroenterology, Cleveland Clinic, Cleveland, OH; 2Gastroenterology & Hepatology, Minnesota Gastroenterology, Minneapolis, MN
INTRODUCTION
Limited short-term readmissions data following hospitalization for Roux-en-Y gastric bypass (RYGB) is available. Given Centers of Medicare and Medicaid Services' push toward bundled payment over 90-days, it is becoming increasingly important to study readmission rates within this period. We report 90-day readmission rates following RYGB, assess trends in readmission rates and factors associated with readmission. Finally, we develop a readmission risk-stratification tool.
METHODS
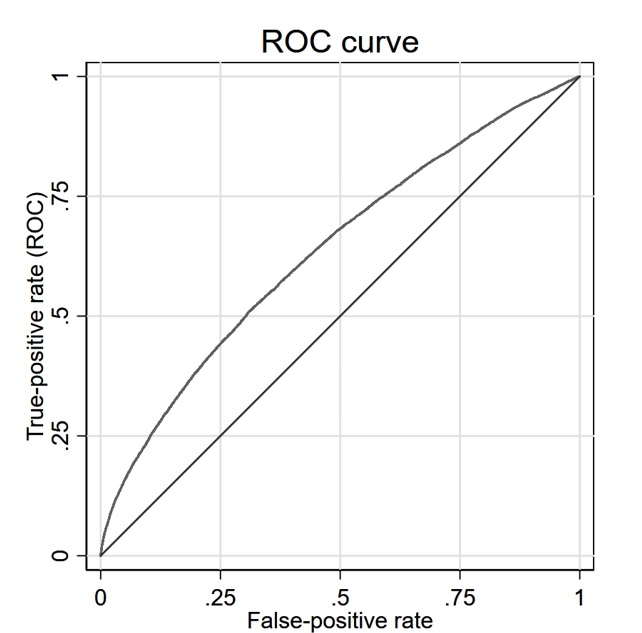
We interrogated the National readmission database (NRD), the largest all-payer readmission database in the US, to identify all patients who underwent RYGB between 2010 and 2014. We assessed 90-day readmission rates as well as trends over the study period. We also identified factors associated with readmission. Finally, we performed forward stepwise logistic regression to develop a risk stratification tool for readmission. Area under the receiver operating characteristics (AUROC) curve was calculated to assess the predictive ability of the model and internal validation was achieved using boot-strapped methods.
RESULTS
N=246,408 hospitalizations resulted in 26,154 (10.6%) readmissions within 90-days. Readmission rate for each year between 2010-2014 were 10.9%, 10.9%, 11.1%, 10.2%, and 9.7% respectively. Surgical complications were the most common reason for readmission (6.6%) followed by gastrointestinal ulcers or hemorrhage (2.1%), fluid or electrolyte imbalance (1.7%), abdominal pain (0.9%), and intestinal obstruction (0.9%). Increasing age, living in zipcodes associated with top quartile of income, non-urban location (patient), elective index admissions, index admission at a teaching hospital, urban location of hospital, and having cholecystectomy performed on index admission were all associated with reduced odds of readmission. Medicare insurance, being a resident of the same state as the hospital, weekend admission, increasing length of stay, hospitalization at a high-volume hospital, discharge with home care, number of chronic diseases, heart or kidney disease, and hernia repair during index admission were all associate with increased risk of readmission (Table 1). AUROC was 0.637 (95%CI, 0.630, 0.643), with boot-strap validation yielding similar AUROC.
CONCLUSION
Ninety-day readmission rate after RYGB is substantial with a slight decrease in trends from 2010 to 2014. Surgical complications are the most common reason for readmission. We developed a risk-stratification tool that identifies patients with a high risk of readmission. By identifying patients with a higher likelihood of readmission, targeted interventions can reduce readmission rates.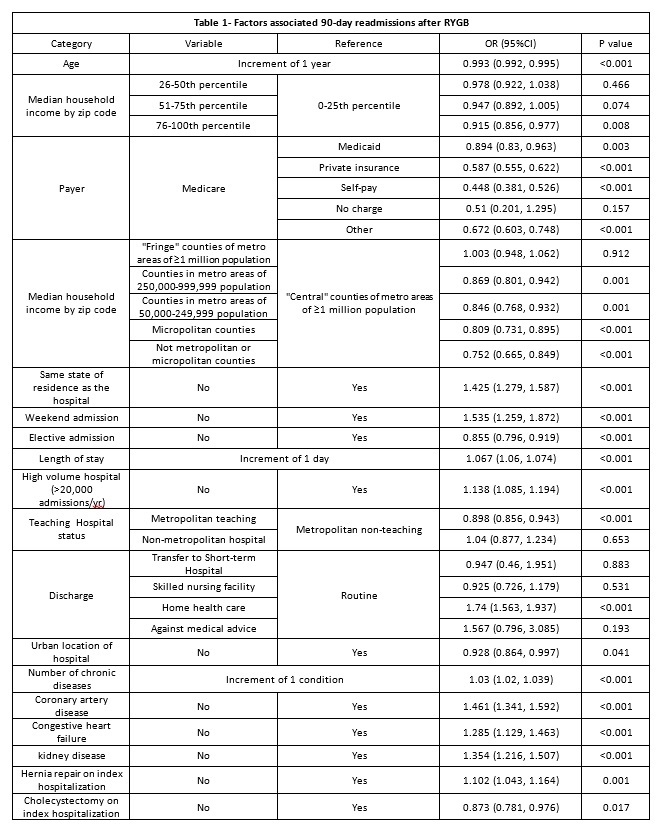
Back to 2019 Posters




