CANCER STAGE INFLUENCES SHORT-TERM OUTCOMES FOR GASTROINTESTINAL CANCER SURGERIES
John Bliton*, Michael K. Parides, John C. McAuliffe, Peter Muscarella, Haejin In
Montefiore Medical Center, Bronx, NY
Background
Surgical outcomes are often examined with consideration for disease-related factors (i.e. location, pathology, complicating factors such as perforation) and patient-related factors (i.e. age, comorbidities). While analysis of long-term outcomes for cancer surgery takes stage into consideration, stage is often not considered when analyzing short-term outcomes. The purpose of this study was to investigate whether cancer stage influences short-term outcomes for gastrointestinal (GI) cancers by examining the effect of cancer stage on 30-day mortality for cancers of the stomach, pancreas, colon, and rectum.
Methods
Analysis was conducted using data from the National Cancer Database (NCDB) of patients from years 2004-2015 who had resections for cancers of the stomach, pancreas, colon or rectum. Descriptive statistics were used to compare the patients' demographics, comorbidities, operation type, hospital factors and tumor characteristics by primary tumor site and stage. Generalized linear mixed models were used to evaluate the relationship between stage and 30-day mortality, controlling for tumor characteristics, operative factors, other patient factors and hospital factors. Pseudo R-square statistics (%ΔR2) were used to quantify the relative explanatory capacity of the variables to the model for 30-day mortality. All analyses were performed using SAS 9.4 (Cary, NC).
Results
Overall, 363,666 patients were included in the analysis (31,735 stomach cancer, 25,124 pancreatic cancer, 224,140, and 72,667 rectal cancer). Patients with higher stages of cancer had higher 30-day mortality. After adjusting for other variables, 30-day mortality was statistically different by stage of cancer for all cancers examined. For example, compared to stage I, stage II disease was associated with higher 30-day mortality; OR 1.42 (95% CI 1.21-1.67), 1.21 (95% CI 1.06-1.38), 1.68 (95% CI 1.58-1.79), and 1.60 (95% CI 1.24-1.93) for stomach, pancreas, colon, and rectum cancers, respectively. Similarly, stage III and stage IV were associated with higher 30-day mortality than stage I. Among pre-operative variables, age (%ΔR2 range 15-24%) and stage of cancer (%ΔR2 range 8-35%) were the two strongest drivers of 30-day mortality for stomach, colon and rectal cancers. For pancreatic cancer, stage was a minor driver of 30-day mortality compared to other factors such as type of surgery and hospital volume.
Conclusion
Stage of cancer influences short-term surgery outcomes for GI cancers. Although the operation performed may be the same for different stages of disease, our analysis shows there is increased 30-day mortality for higher stages of disease, particularly for stomach, colon and rectal cancers. Cancer stage should be considered for analyses on short-term outcomes following cancer surgery.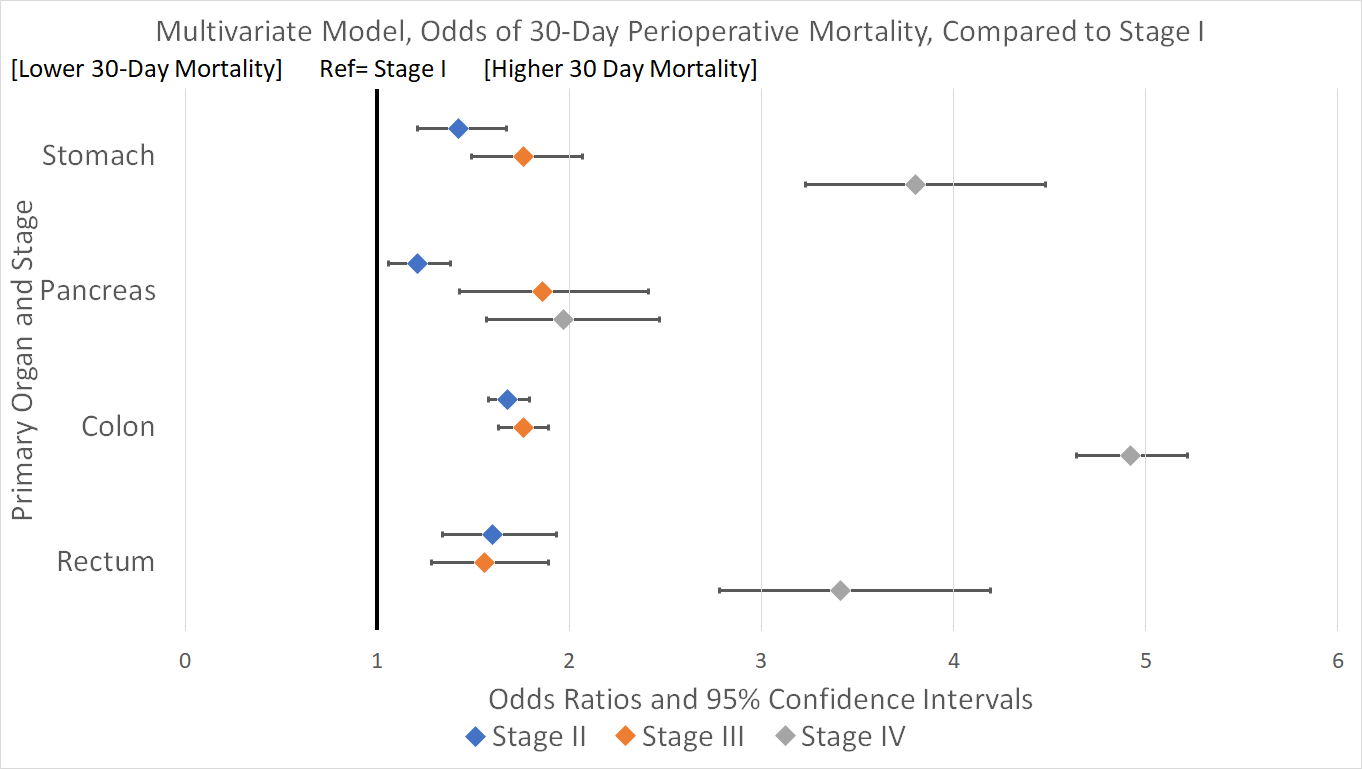
Back to 2019 Posters




