DOES LAPAROSCOPIC VERSUS OPEN APPROACH AFFECT PREDICTIVE ABILITY OF C-REACTIVE PROTEIN TO DETECT ANASTOMOTIC LEAKS IN COLORECTAL SURGERY? A SYSTEMATIC REVIEW AND META-ANALYSIS
Tiffany Paradis*1, Anudari Zorigtbaatar1, Maude Trepanier1,2, Tara Landry3, A. Sender Liberman2, Patrick Charlebois2, Barry Stein2, Gerald M. Fried2,1, Liane S. Feldman2,1, Lawrence Lee2,1
1Steinberg-Bernstein Centre for Minimally-Invasive Surgery and Innovation, McGill University Health Centre, Montreal, QC, Canada; 2Department of Surgery, McGill University Health Centre, Montreal, QC, Canada; 3Medical Libraries, McGill University Health Centre, Montreal, QC, Canada
Introduction: Early identification of complications after colorectal surgery may allow for improved outcomes. C-reactive protein (CRP) is an inflammatory marker that has been previously shown to predict postoperative morbidity after colorectal surgery. However, past analyses did not differentiate between laparoscopic and open surgery. Laparoscopy may minimize surgical inflammatory response and potentially alter the diagnostic characteristics of CRP. Therefore, the objective of this study was to perform a systematic review and meta-analysis on the diagnostic characteristics of CRP to detect anastomotic leaks and infectious complications after laparoscopic and open colorectal surgery.
Methods: A systematic review was performed according to PRISMA guidelines of Medline, Embase, CENTRAL, DARE, PubMed, Scopus, ClinicalTrials.gov, and WHO International Clinical Trials Registry Platform. Studies were included if they reported on the diagnostic characteristics (CRP threshold, sensitivity, and specificity) of postoperative day (POD) 3-5 values of serum CRP to diagnosis anastomotic leak or infectious complications specifically in patients undergoing elective laparoscopic and open colorectal surgery. The main outcome for meta-analysis was a composite of anastomotic leak and infectious complications. CRP thresholds were pooled using geometric means. A random-effects model was used to perform a meta-analysis of diagnostic accuracy characteristics (area under the curve (AUC), sensitivity, and specificity). The trial protocol was registered in the PROSPERO registry.
Results: Out of 1070 unique citations, 166 studies underwent full-text review and 13 were included for meta-analysis. There were 9 studies reporting diagnostic characteristics after laparoscopic surgery, and 8 for open surgery. The mean sample size in the laparoscopic studies was 417 (range 71-1187) and 200 (range 80-468) in open studies. The pooled incidence of the composite outcome was 14.8% (95%CI 10.2, 19.3) in laparoscopic studies and 21.0% (95%CI 11.9, 30.0) for open. Only one study reported diagnostic characteristics specifically for proctectomy. The pooled AUC, sensitivity, and specificity of CRP to detect the composite outcome was similar for open and laparoscopic studies for POD 3, 4, and 5 (Table). However, the CRP threshold cut-offs were lower in laparoscopic studies for POD 3 and 4, but similar on POD 5 (Table).
Conclusions: The diagnostic characteristics of POD 3 to 5 CRP to detect infectious complications and leaks after laparoscopic and open colorectal surgery are similar. However, CRP thresholds on POD 3 and 4 are lower for laparoscopic surgery, suggesting that the interpretation of serum CRP values need to be tailored based on operative approach.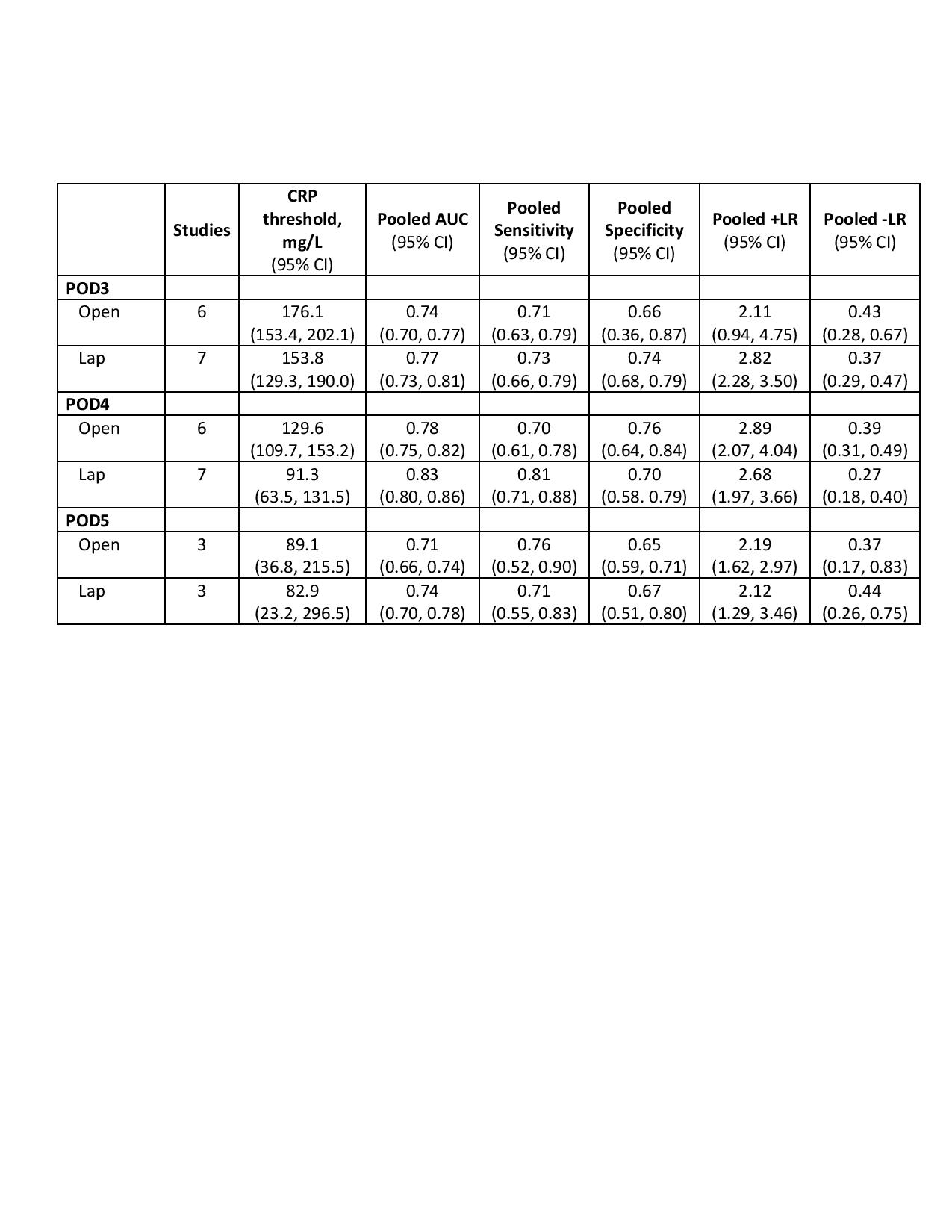
Back to 2019 Posters




