EMERGENT VERSUS ELECTIVE OSTOMIES FOR COLON CANCER: IS THERE A DIFFERENCE?
Hannah M. Thompson*1, Maria Altieri2, Jie Yang1, siao sun1, Jill Genua1, Aurora D. Pryor1
1Surgery, Stony Brook University, Stony Brook, NY; 2Surgery, Washington University School of Medicine, St. Louis, MO
Background: Many patients undergoing colon resection for colon cancer have a temporary ostomy placed; however, not all these patients will eventually have a reversal. The aim of the current study is to examine the rate of ostomy reversal amongst patients who undergo temporary ostomy creation in an elective versus emergent setting.
Methods: Using the New York State SPARCS longitudinal administrative database, all adult patients undergoing colon resection were identified between 2000 and 2011. Through the use of ICD-9, ICD-10, and CPT codes, patients with temporary ostomy creation for colon cancer were then followed until 2016. Cox proportional hazard model was used to compare ostomy reversal after adjusting for patients' demographics, co-morbidities and complications at the time of ostomy.
Results: There were 11,335 patients who underwent a colon resection with ostomy creation during the studied period. From these patients, 5,122 (45.19%) subsequently had an ostomy reversal with the majority (n=3543, 69.17%) being created in the elective setting. Median time to reversal was 158 +/- 157 days (IQR) for elective ostomies and 185 +/- 216 days (IQR) for emergent ostomies among all ostomy reversal patients. Patients who underwent ostomy creation in an elective setting were more likely to have ostomy reversal (adjusted HR=1.92, 95% CI: 1.80-2.05, p-value<0.0001). Furthermore, there was a significant difference in cumulative incidence (Figure 1) which suggests a higher incidence at any time point of ostomy reversal amongst elective colon resections with ostomy creations than emergent procedures. In addition, Caucasian race compared to African American and Hispanic was associated with higher rate of ostomy reversal (adjusted HR= 1.35, 95% CI: 1.21-1.51, adjusted HR=1.16, 95% CI: 1.03-1.32, respectively). Patients with Medicaid vs Medicare had a lower rate of ostomy reversal (adjusted HR= 0.82, 95% CI: 0.72-.94). Finally, the incidence of a complication at the time of ostomy creation was not found to be associated with ostomy reversal.
Conclusion: Ostomy reversal rates are impacted by the setting in which the original colon resection and ostomy creation take place. Additionally, patient's racial and socioeconomic backgrounds appear to play a factor in ostomy reversal. There are opportunities for further studies to elucidate the barriers to ostomy reversal amongst patients undergoing emergent stoma creation, as well as, barriers facing Medicare and Black and Hispanic patients.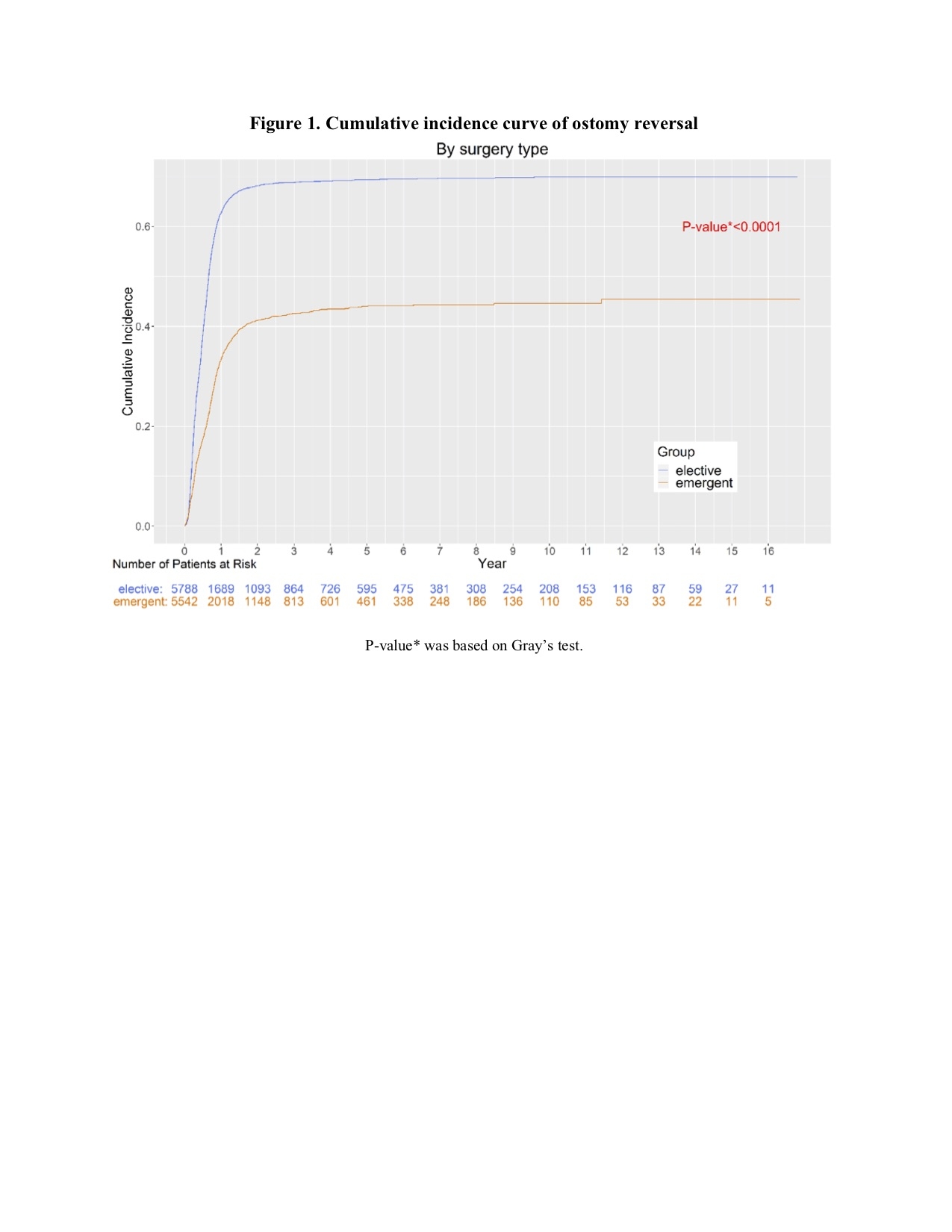
Back to 2019 Posters




