STUCK BETWEEN A ROCK AND A HARD PLACE
Juan Ricardo*, Talal Alkayali, Ahmed I. Salem, Belissa M. Ramos Chaves, Jorge Conte
Florida State University College of Medicine, Sarasota Memorial Hospital, Sarasota, FL
Introduction: Cholecystoenteric fistula (CEF) is a rare complication of biliary disease, notably in the setting of cholelithiasis, neoplasia, or post-operative hepatobiliary interventions. A high index of suspicion and early diagnosis are crucial as these fistulas can have myriad clinical presentations and consequences.
Case: A 72-year-old Caucasian female presented to the ER with 3-days of abdominal pain that started after ingestion of pizza. She described pain as sharp, epigastric and right upper quadrant, and radiating to back. The pain was associated with nausea, nonbloody/nonbiliary emesis and anorexia. She denied fever, rigors, and changes in bowel habits. Past medical history significant for GERD, hyperlipidemia, hypothyroidism, diverticulitis and sigmoid colectomy. Medications included Pantoprazole, Atorvastatin, and Levothyroxine.
Physical Exam: Vital signs normal. Obese patient in moderate distress. Anicteric, abdomen was nondistended, with normal bowel sounds, epigastric and RUQ tenderness to deep palpation, positive Murphy sign. Absent rebound, guarding, or palpable masses. Other systems unremarkable.
Laboratory/Imaging Studies: Normal CBC, BMP, lipase, hepatic function panel including bilirubin. Abdomen XR showed normal bowel gas pattern. CT of Abdomen/Pelvis with IV, w/o PO contrast revealed cholecystoduodenal fistula extending from the gallbladder neck to the duodenum with pneumobilia within inflamed gallbladder (Figure 1). A large 4 cm gallstone eroded into the duodenum (Figure 2).
No clinical signs of infection were present to warrant antibiotics. Open cholecystectomy was performed. A large gallstone noted within the duodenal bulb was extracted. A cholecystoduodenal fistula of 1 cm lengthand thickened from chronic inflammation was repaired and biopsied. A gastrojejunostomy tube was inserted, along with two separate drains from the duodenum. Patient was discharged after tolerating oral intake following removal of drains and feeding tube. Biopsies returned negative for malignancy.
Discussion: Cholecystoenteric fistula(CEF) has an incidence of 0.9%. Risks factors include large gallstones, recurrent cholangitis, female sex, and age >60 years. CEF is caused by inflammation associated with acute cholecystitis, peptic ulcer, or malignancy between gallbladder and a portion of intestine. CEF may also occur with pressure necrosis from impaction of a gallstone and its subsequent erosion through the gallbladder and duodenal wall. The most common communication is between the gallbladder and duodenum, followed by cholecystocolic and cholecystogastric fistula. While ultrasound can reveal contact between gallbladder and inflamed intestinal wall, CT-scan is the recommended imaging modality to investigate the presence of CEF-though it is often diagnosed intraoperatively. Laparoscopic management of cholecystoenteric fistula is the treatment of choice.
Cholecystoduodenal fistula (Thick arrow) with pneumobilia (Thin arrow). Large gallstone within the duodenum (Star).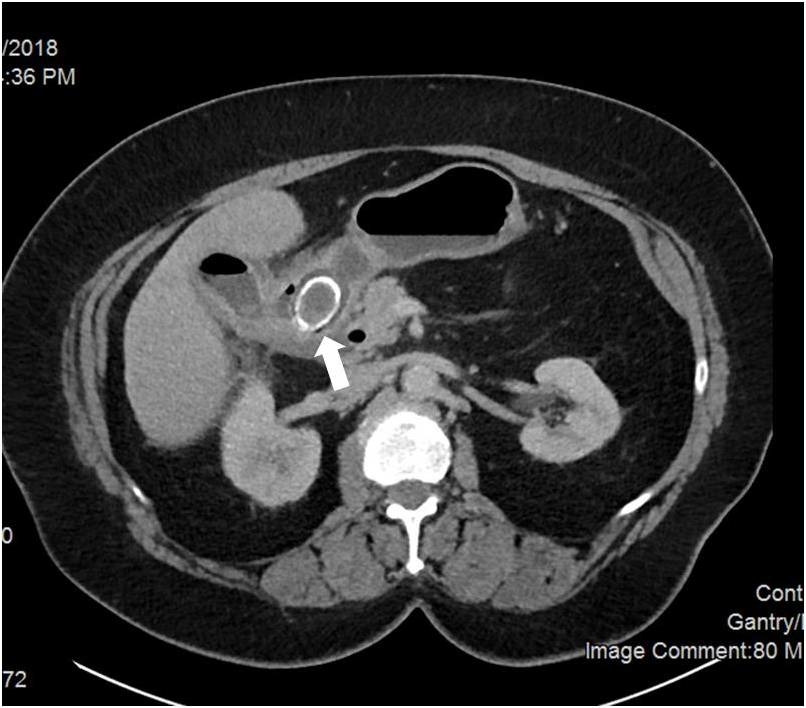
Large 4 cm gallstone eroded into the duodenum (Arrow).
Back to 2019 Posters




