SHOULD WE PERFORM CHOLECYSTECTOMIES ON PATIENTS WITH BLOOD CANCERS?
Camille Stewart*1, Andrew H. Nguyen1, Jasmine Zain2, Lily Lai1, Yuman Fong1, Yanghee Woo1
1Surgery, City of Hope, Duarte, CA; 2Hematology & Hematopoietic Cell Transplantation, City of Hope, Duarte, CA
Background: Surgeons are intermittently asked to perform cholecystectomies on patients with hematologic malignancies who are often immunosuppressed and thrombocytopenic. Operating on these patients is anxiety provoking. We sought to characterize our experience to determine outcomes and inform future practice.
Methods: We queried the electronic medical record for patients with hematologic malignancies who had a cholecystectomy for benign biliary disease from 1/1/2012 - 8/1/2018.
Results: We identified 49 patients with hematologic malignancies who had a cholecystectomy for benign biliary disease. Most were taking antibiotics (38/49, 78%) and immunosuppressive medication (44/49, 90%) at consultation; many were status post bone marrow transplant (33/49, 67%). Nearly all had symptoms (47/44, 96%), typically pain (44/49, 90%). There were 22/49 (45%) who had surgery electively, and 27/49 (55%) who had surgery while already inpatient, 9/27 (33%) after a course of antibiotics. Surgical time was 1:37 +/- 00:35 (range 00:40 - 3:10), estimated blood loss was 95 ± 146 mL (range 5 - 800 mL), 9/49 (18%) required a peri-operative transfusion, and drains were placed in 16/49 (33%). Laparoscopic cholecystectomy was converted to open in 5/47 (11%). Operative time, estimated blood loss, and need for transfusion did not differ between patients operated on immediately, after a course of antibiotics, or electively. Patients thrombocytopenic at consultation (platelets <100, n=15) more frequently required peri-operative transfusions (40% vs. 9%, p=0.009), but similar length of stay after surgery. Patients who were anemic at the time of consultation (hemoglobin <10, n=20) also more frequently required peri-operative transfusions (40% vs. 3%, p=0.002), but did have longer length of stay after surgery (p=0.004, figure). For patients treated electively, 8/22 (36%) had surgery performed as an outpatient, and 10/22 (45%) were hospitalized over night. There were 8/49 (16%) complications - half grade III or higher, and no deaths.
Conclusions: Cholecystectomy can be performed on patients with hematologic malignancies with relative safety and as an outpatient in select individuals. Timing is patient specific, and does not seem to affect operative time or estimated blood loss. Many require transfusions and drains.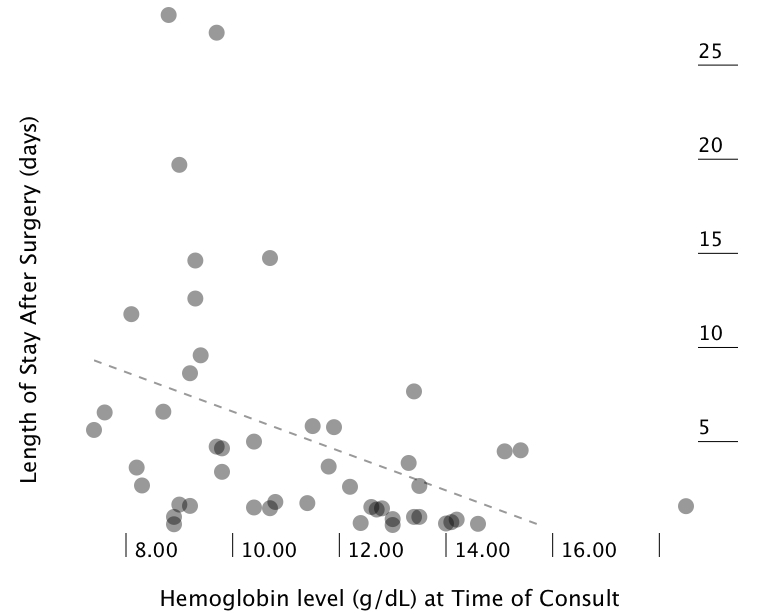
Back to 2019 Posters




