IMPACT OF AGE ON SHORT- AND LONG-TERM OUTCOME AFTER PANCREATODUODENECTOMY
Mario Gruppo*, Francesca Tolin, Genny Mattara, Luca Pomba, Pierluigi Pilati
Unit of Surgical Oncology of the Esophagus and Digestive Tract, Veneto Institute of Oncology IOV-IRCCS, Padua, Italy
BACKGROUND: Although mortality and morbidity of pancreatoduodenectomy (PD) have improved significantly over the past years, the impact of age for patients undergoing PD is still debated. This study aimes to analyze short- and long-term outcomes of PD in elderly patients.
METHODS: 124 consecutive patients, undergone PD for periampullary neoplasms in our center between 2012 and 2017, were analyzed. Patients were divided into two groups: group I (<70 years), group II (≥70 years). Demographic features, intraoperative and clinic-pathological data were collected. Primary endpoints were postperative morbidity and mortality; complications were classified according to Clavien-Dindo score. Secondary endpoints included feasibility of adjuvant treatment and overall survival rates.
RESULTS: A total of 106 patients were included in this study. There were 64 (60.4%) patients in group I and 42 (39.6%) in group II. Perioperative deceases were 4 (3.6%), postoperative pancreatic fistulas were 34 (32,1%). Demographic, intraoperative and clinic-pathological features of two groups are summarized in table 1. Significant difference was demonstrated for ASA score, pancreas consistency, Karnofsky index, preoperative jaundice. 68,7% of patients in group I underwent adjuvant treatment vs 40,6% of older ones (p=0,012). Mean overall survival was 26 months in group I vs 21,1 months in group II (p=0,8) (Fig.1).
CONCLUSIONS: PD can be performed safely in elderly patients. Advanced age should not be a contraindication for PD. The outcome of elderly patients who have undergone PD is similar to that of younger patients, even though adjuvant treatment administration is significantly lower, demonstrating that surgery remains the main therapeutic option.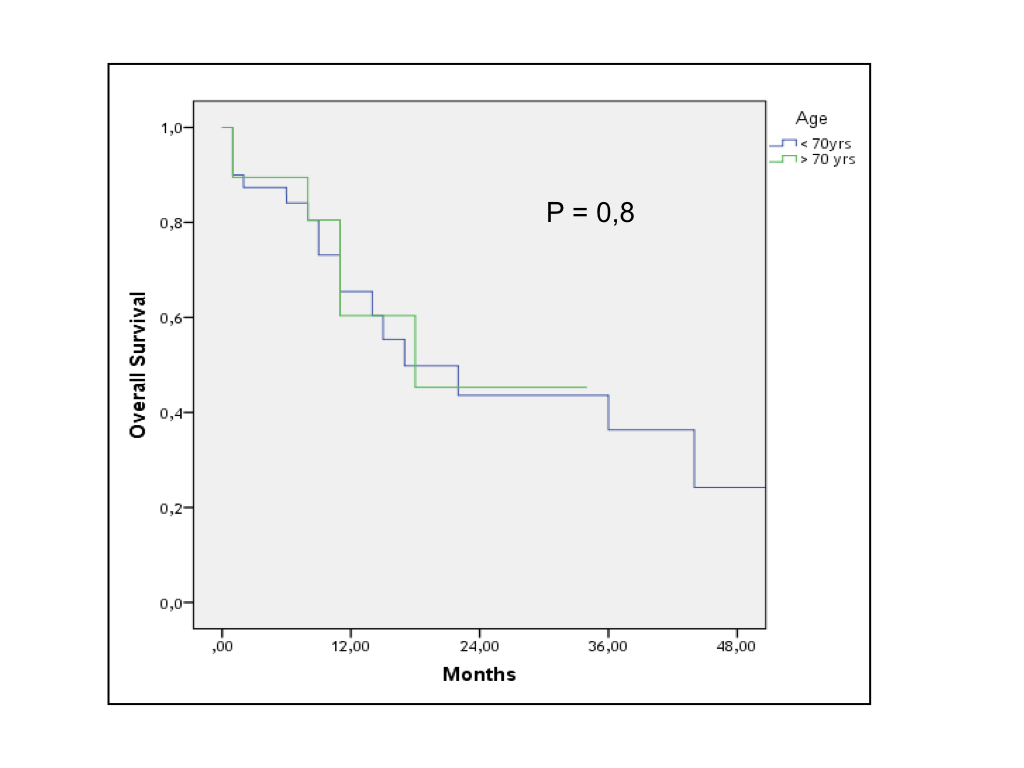
Figure 1. Overall survival of 106 patients according to age stratification.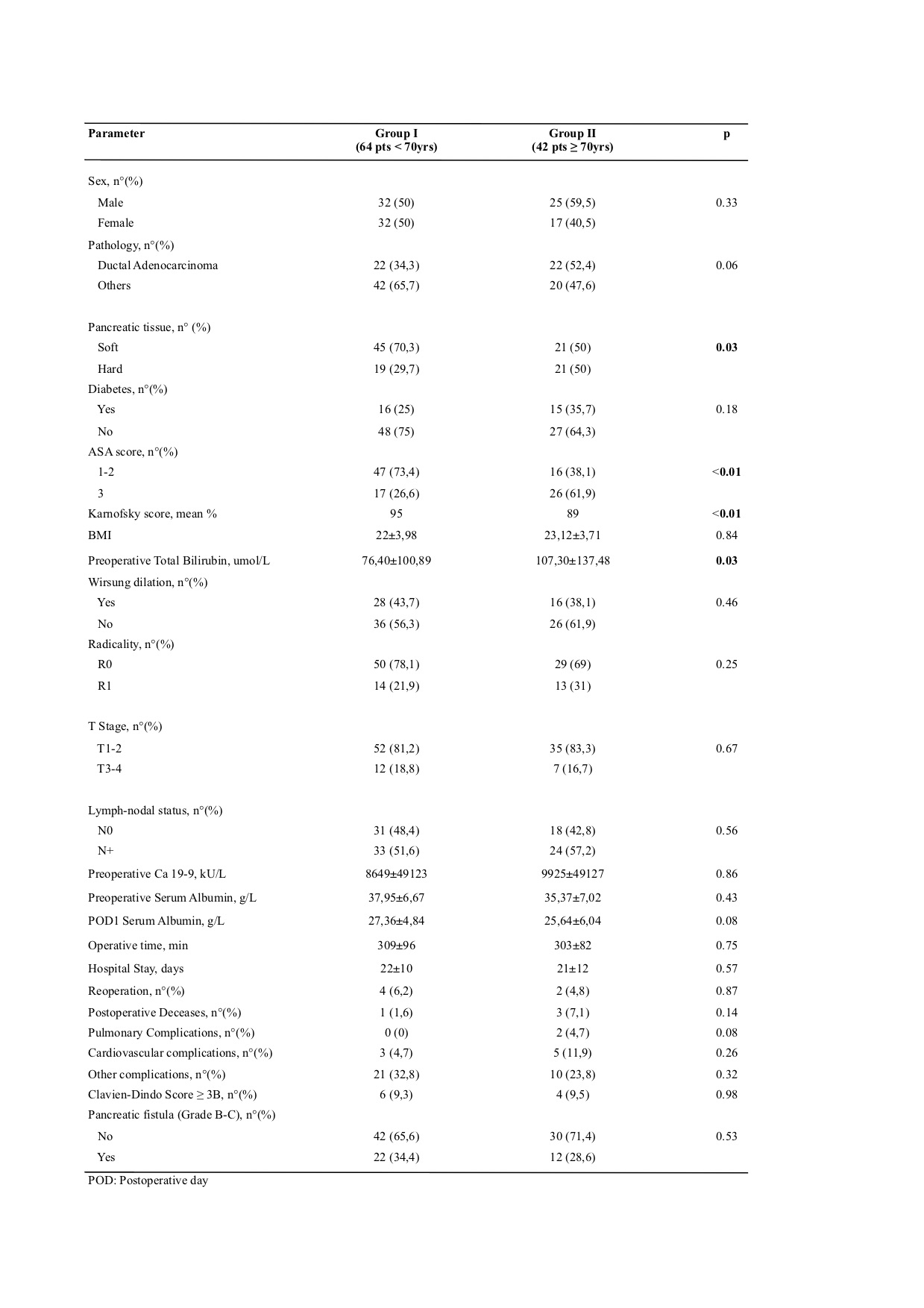
Table 1. Demographic, intraoperative and clinico-pathological parameters of 106 patients
Back to 2019 Posters




