LAPAROSCOPIC VS OPEN DISTAL PANCREATECTOMY FOR ADENOCARCINOMA OFFERS COMPARABLE OUTCOMES
Eduardo A. Vega3, Onur C. Kutlu*1, Sandeep Krishnan4, Jeffrey Wisch2, Frank Pomposelli5, Dicken Ko6, Danny Sleeman1, Nestor de La Cruz1, Claudius Conrad6
1Surgery, University of Miami, Miami, FL; 2Dana-Farber Cancer Institute, Boston, MA; 3Surgical Oncology, UT MD Anderson Cancer Center, Houston, TX; 4Internal Medicine, St Elizabeth's Medical Center, Boston, MA; 5Surgery, Tufts University, Boston, MA; 6Surgery, St Elizabeth's Medical Center, Boston, MA
Introduction:
Clinical outcomes of laparoscopic distal pancreatectomy (LDP) is well studied for benign processes. Concerns exists whether the quality of oncologic resection using LDP in pancreatic adenocarcinoma is comparable to open distal pancreatectomy (OPD). This study compares the perioperative outcomes and adherence to oncologic surgical standards as a function of surgical approach.
Material and methods:
National Cancer Database was queried for patients diagnosed with pancreatic adenocarcinoma, who underwent distal pancreatectomy between 2010-2014. Only cases with known age, sex, comorbidities, N-stage, grade, tumor size, T-stage, margin status, surgical approach, chemotherapy sequencing, 30 and 90-day mortality, institutional case volume were included. Effect of laparoscopic (LDP) vs open (ODP) and institutional case volumes on margin status, 30 and 90-day mortality, administration of adjuvant chemotherapy (AC), and hospital stay was analyzed by binary and linear logistic regression modelling.
Results:
1355 patients fit inclusion criteria. There were 284 (26.8%) LDP and 1073 (79.1%) ODP. Rates of margin positivity was 21.2% for the entire cohort, 14.7% for LDP and 22.9% for ODP (OR: 1.656, p=0.008). 30-day mortality was 1.2 % for the LDP and 2.2% for ODP. 90-day mortality was 2.3 % for LDP and 4.6% for ODP. After correcting for confounders no significant difference was found between LDP and OPD for 30-day (p=0.124) and 90-day mortality rates(p=0.09). The rates of AC were 62% in the LDP and 59% in the ODP group (p=0.64). Rates of delay to chemotherapy >90 days were 11.6% in the LDP and 10.2 in the ODP group (p=0.129). Median hospital stay was 6 days in the LDP and 8 days in the ODP group (p=0.007).
Conclusion:
LDP is an effective and oncologically safe alternative to ODP in the management of pancreatic adenocarcinoma. However, LDP leads to similar shorter recovery and higher probably of receiving AC in higher volume institutions.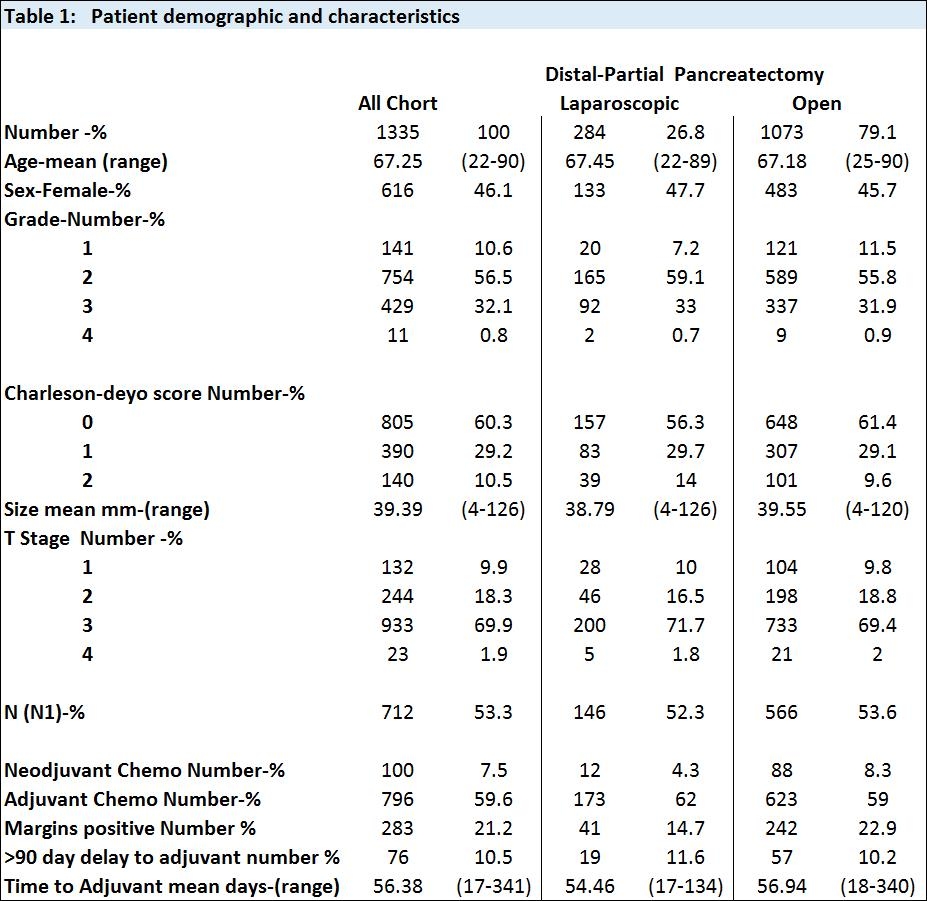
Back to 2019 Posters




